Cluster Headache
Many chronic conditions are challenging to manage. Here we focus on key pain conditions with a high unmet need among patients and/or healthcare professionals.
Our aim here is to provide the pain community with in-depth information about these conditions; from disease understanding to management approaches.
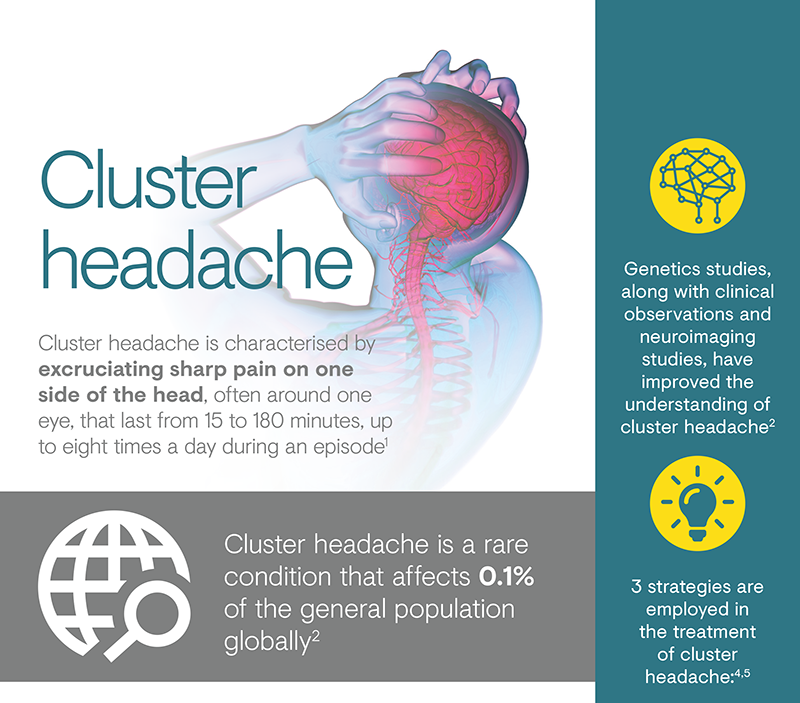
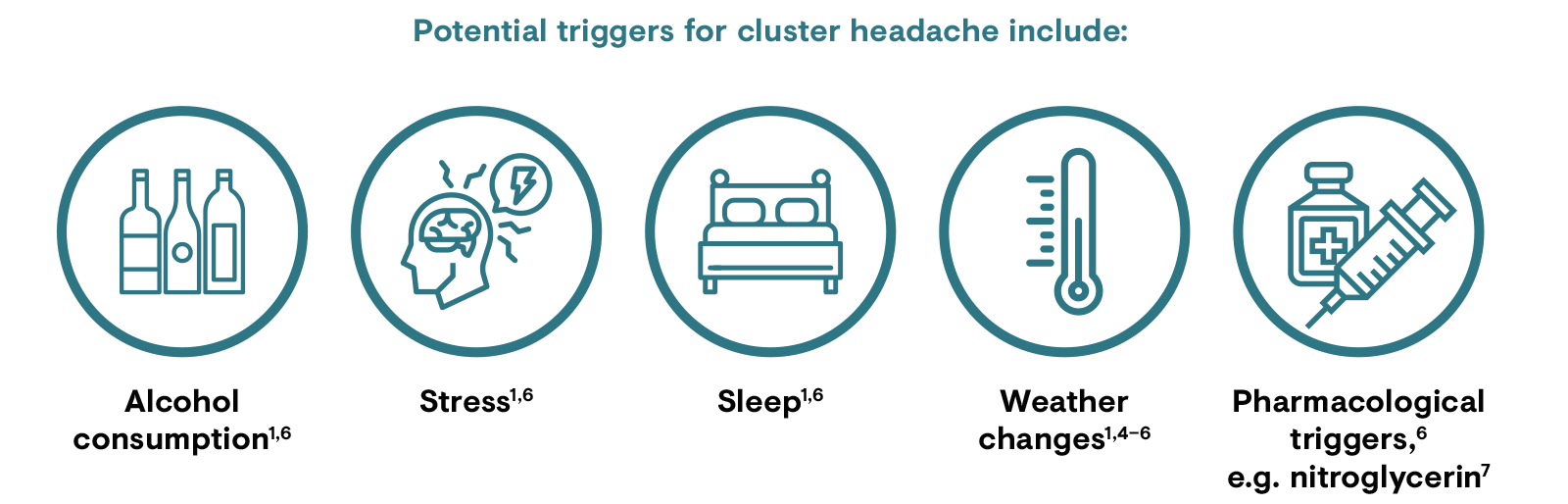
Cluster headache has been described as the most painful condition in humans.1,3 It is characterised by excruciating sharp pain on one side of the head, often around one eye, that lasts from 15 to 180 minutes, up to eight times a day during an episode.3 Cluster headache can be episodic (occurring for periods lasting from 7 days to 1 year, separated by pain-free periods of at least 3 months) or chronic (lasting for 1 year or longer without remission or with remission periods less than 3 months at a time).3 The appearance of cluster headache is often seasonal, focused particularly around the clocks changing to daylight saving time, and they will often occur around the same time each day.1,4,5
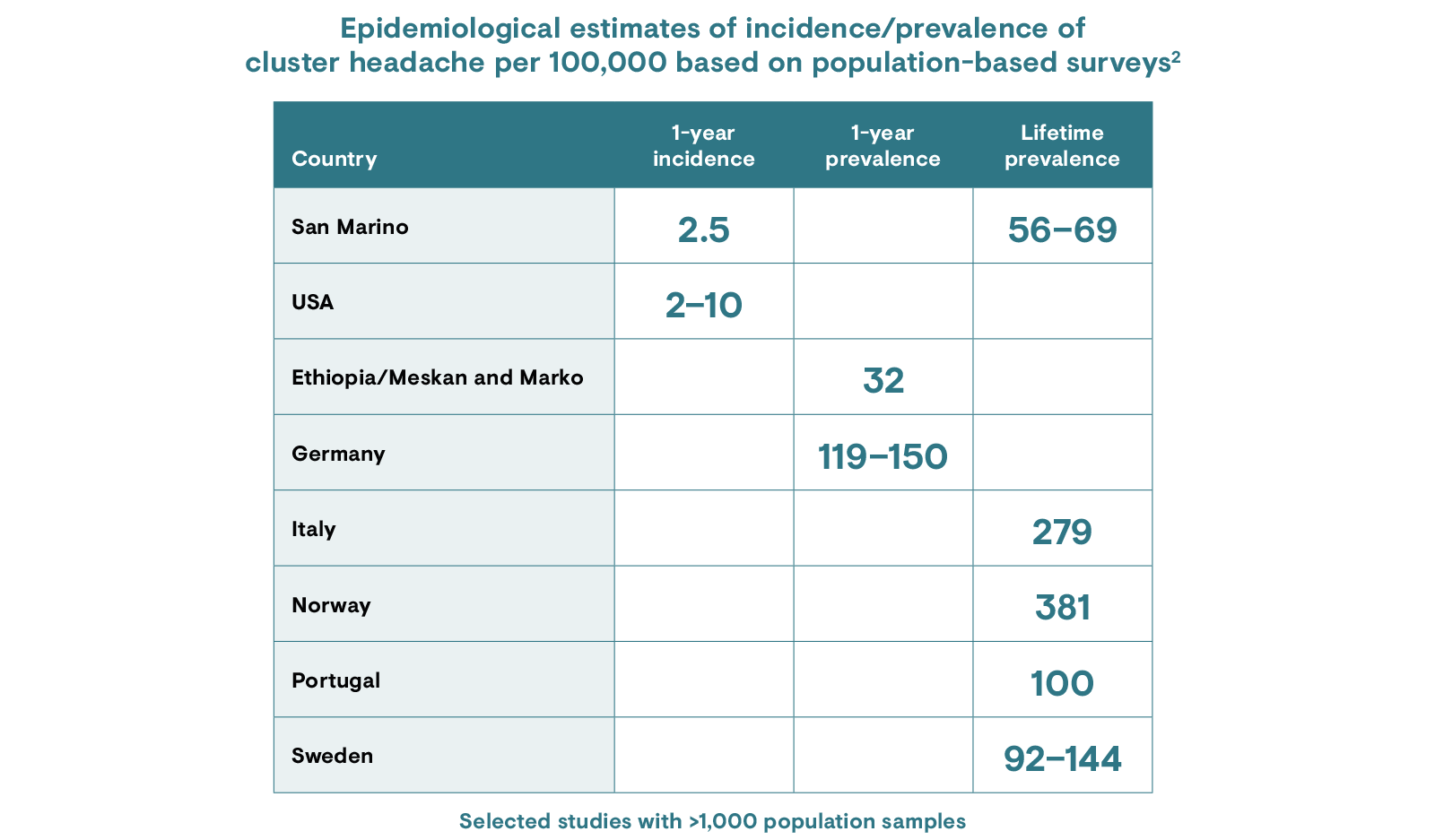
Globally, cluster headache affects 0.1% of the general population, with an onset ranging from 10 to 68 years.1 It is more common among men than women, with men being 4.3 times more likely to suffer from cluster headaches.2 The episodic form is more common than the chronic form and affects 80–90% of patients with cluster headache.1
Cluster headache can run in families, although it is difficult to pin down genetic factors in this disease as it is very complex and has a low prevalence.1 Other risk factors include male sex and modifiable lifestyle choices.1,3

Cluster headache attacks and attack periods often display an intriguing seasonal and/or circadian rhythmicity, with peaks in the spring and autumn and attacks occurring around the same time each day.4,5 It is postulated that abnormalities in the hypothalamus, which regulates the body clock, may play a role.4,5
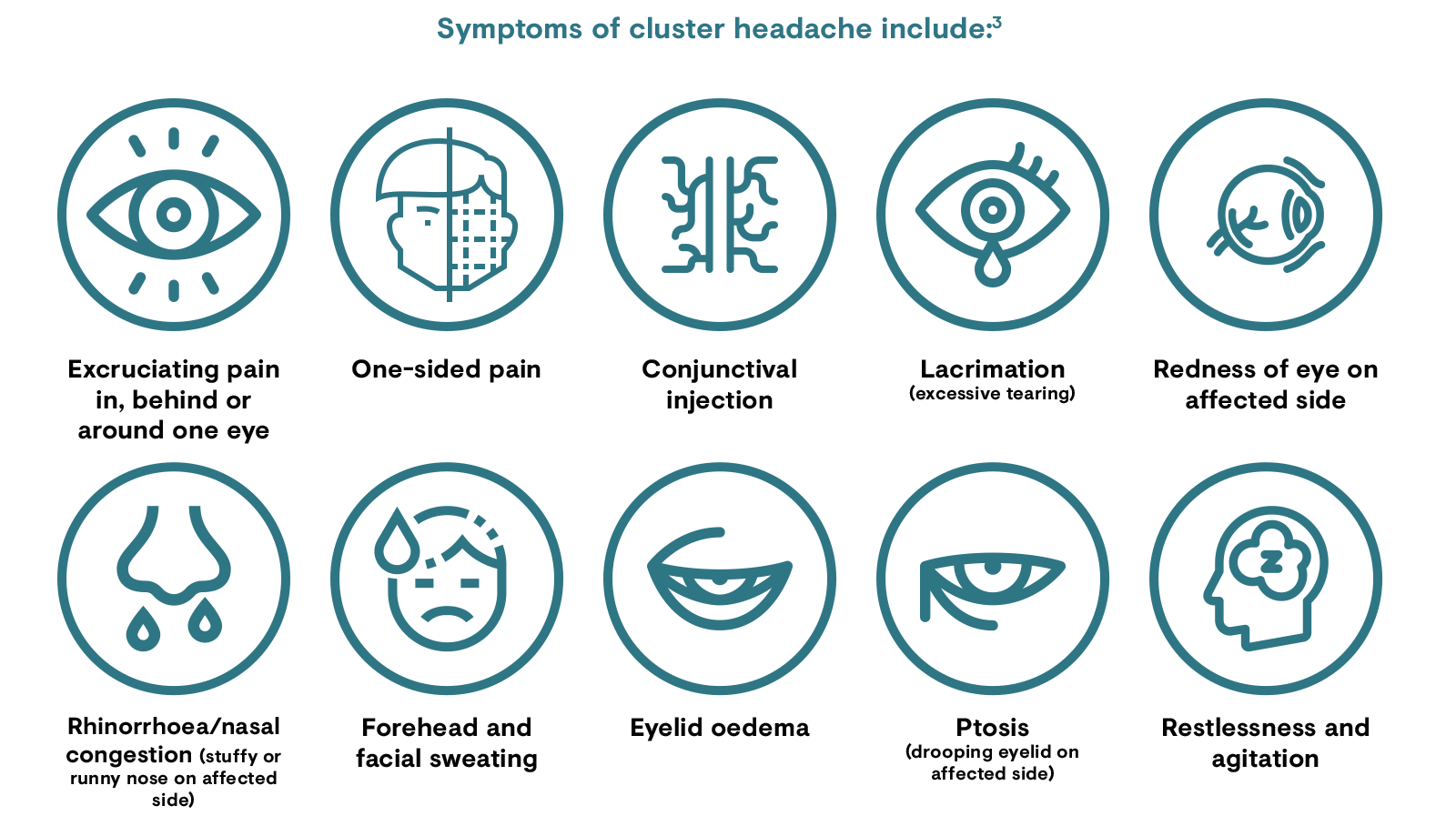
Cluster headache presents as one-sided pain behind or around one eye.3 Recurrent attacks often focus around the same eye.3 Other symptoms include conjunctival injection, lacrimation, redness, rhinorrhoea/nasal congestion, forehead sweating, eyelid oedema, ptosis and restlessness or agitation;3 people with cluster headache are usually unable to lie down and typically pace.3 Cluster headache often occurs in episodes that last for 1 week to 1 year and are followed by a pain-free remission period of up to 12 months.3
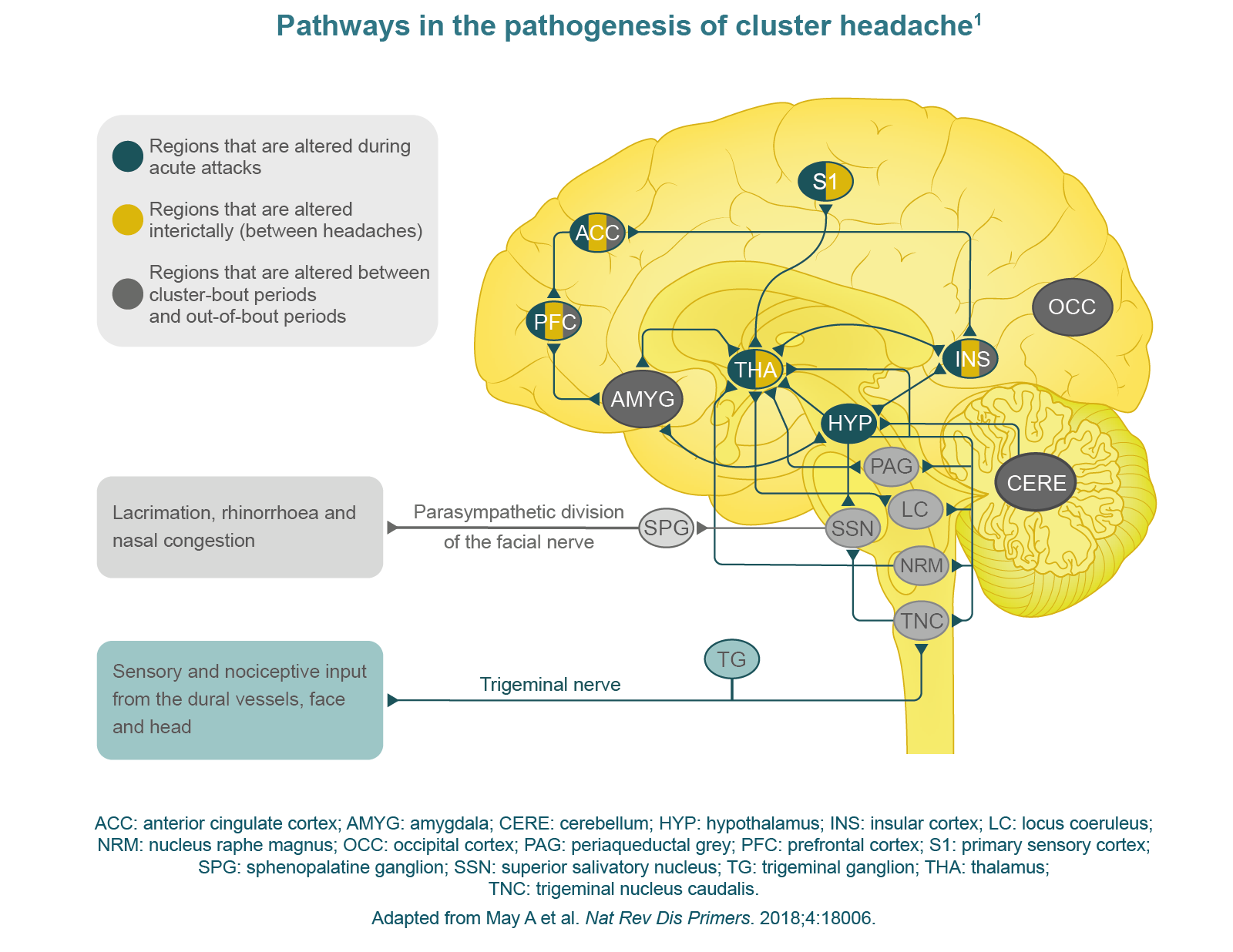
Cluster headache has a complex pathophysiology and the underlying mechanisms are not fully known. Although they present as very different headache disorders, the pathophysiology of cluster headache is similar to that of migraine and the pain in the head is believed to be mediated by activation of neuronal pathways in the trigeminovascular system.1,8 The strongest evidence for alterations in patients with cluster headache is for the hypothalamus, where initial structural and functional changes take place.1 Several neuronal connections exist between the hypothalamus and regions of the trigeminovascular system, with studies indicating that the hypothalamus receives sensory input, including nociceptive information, from areas of the face and cranium innervated by the trigeminal nerve.1
In addition, anatomical and functional links between the hypothalamus and brain areas that are traditionally not considered to be involved in pain processing, such as the occipital cortex and cerebellum, are altered in cluster headache and may have a contributory role in its pathophysiology.1
The autonomic symptoms of cluster headache are thought to be mediated through the trigeminal autonomic reflex, with activation of the trigeminal nerve thought to lead to activation of parasympathetic efferents, producing autonomic symptoms.1
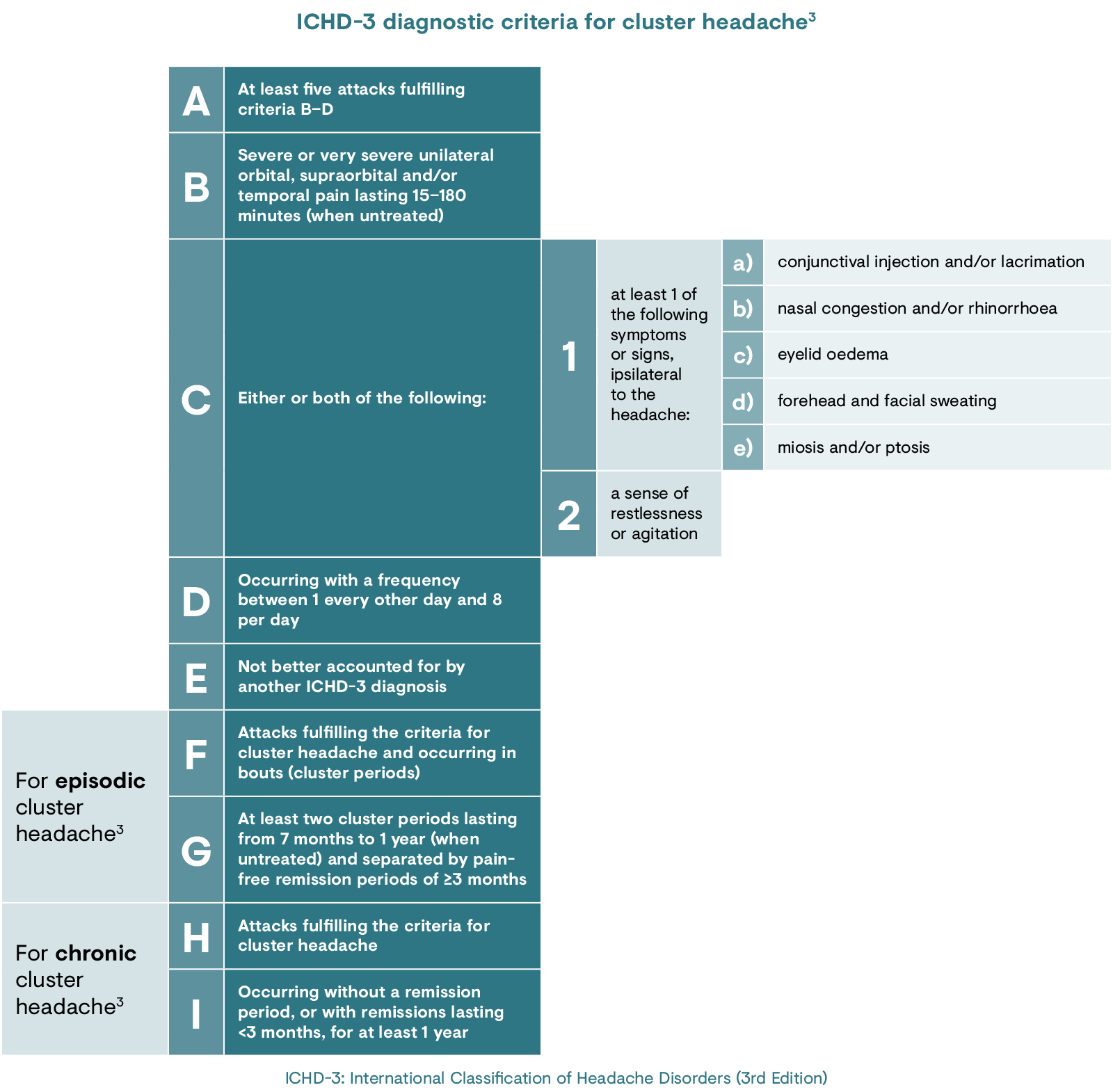
The diagnosis of cluster headache is based primarily on the patient’s
symptoms and involves excluding other primary and secondary
headaches.1 Diagnosis is challenging, and patients often
consult various specialists prior to receiving the final and true
diagnosis.7
There are two types of cluster
headache (as defined by the International Classification of Headache
Disorders [ICHD]-3 diagnostic criteria for cluster headaches), which
are differentiated by their periods of remission between bouts.3
Patients with episodic cluster headache experience pain-free periods
of at least 3 months, while those with chronic cluster headache have
persistent attacks occurring for more than 1 year without remission
or a remission period lasting less than 3 months.3
Once effective treatment has been established, future episodes of cluster headache, or maintenance therapy in the case of chronic cluster headache, can be managed by primary care providers, albeit with frequent follow-up.9 Patients with episodic cluster headache in remission should be advised to return promptly at the onset of the next cluster headache episode.9
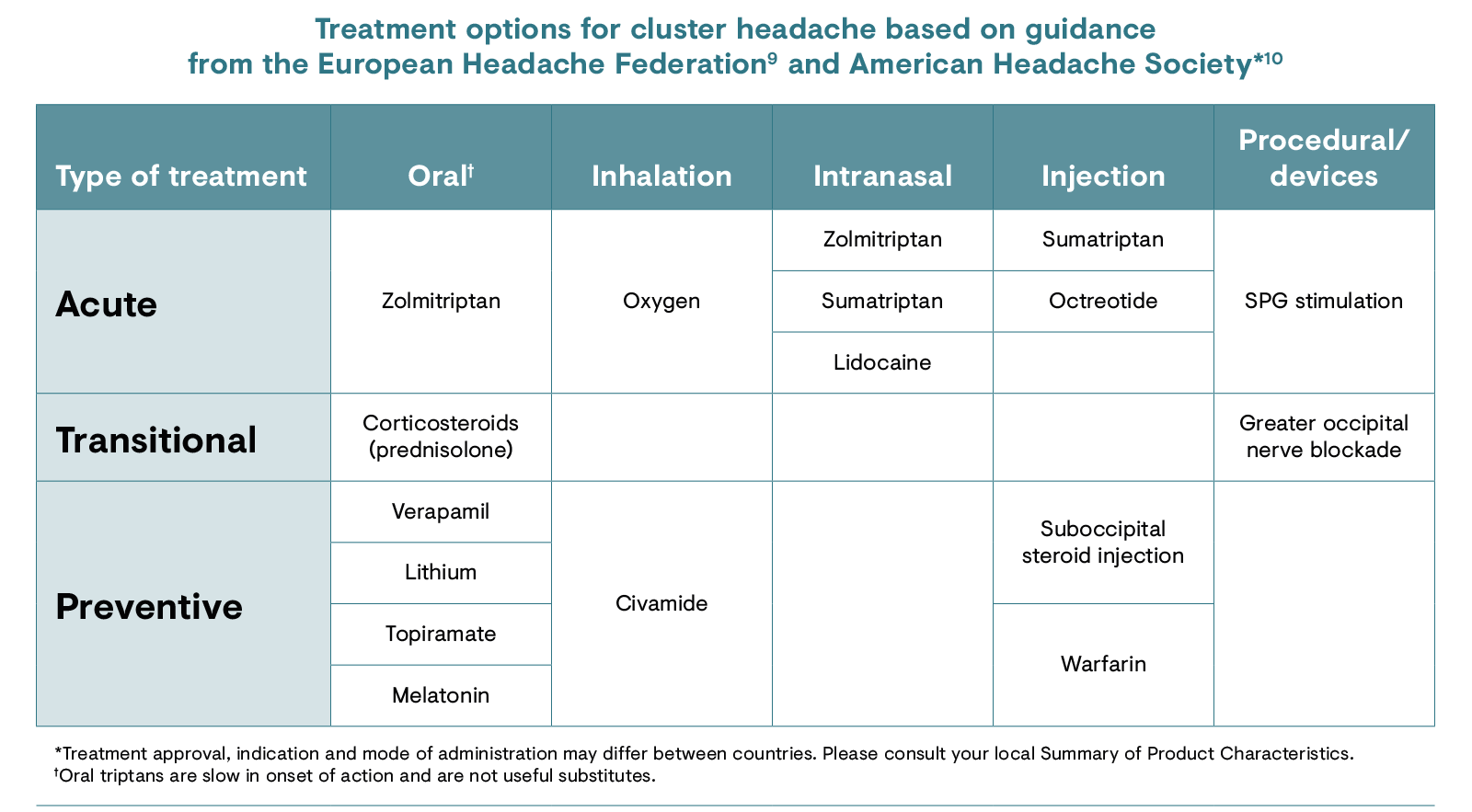
SPG: sphenopalatine ganglion.
Although the objective of management in both episodic and chronic cluster headache is total attack suppression, this is not always achievable.9 Three strategies are employed in the treatment of cluster headache. Acute or abortive treatments are used in individuals attacks to stop the pain once it has started.9 Preventive treatments are used for the duration of the cluster period to reduce frequency, duration and severity of individual attacks within that period, and are the mainstay of treatment in the majority of cases.9 Interim (transition) treatments are given at the onset of a cluster period to achieve more rapid response during dose escalation of any of the preventive drugs and may be used while waiting for a preventive treatment to have a therapeutic effect.9,11
There is a lack of large-scale controlled trials on treatment of cluster headache.1 While genetic studies, clinical observations and neuroimaging studies have improved the understanding of cluster headache,1 further research is necessary to characterise the cause of cluster headache and identify new biomarkers to inform the development of improved treatments.
1. May A et al. Nat Rev Dis Primers. 2018;4:18006.
2. Fischera M et al. Cephalalgia. 2008;28:614–8.
3. International Headache Society (IHS). Cephalalgia. 2018;38:1–211.
4. Naber WC et al. Cephalalgia. 2019;39:1855–66.
5. de Coo IF et al. Headache. 2019;59:1032–41.
6. Vollesen AL et al. J Headache Pain. 2018;19:89.
7. Ljubisavljevic S & Trajkovic JZ. J Neurol. 2019;266:1059–669.
8. Hoffmann J et al. J Cerebr Blood Flow Metab. 2019;39:573–94.
9. Steiner TJ et al. J Headache Pain. 2019;20:57.
10. Robbins MS et al. Headache. 2016;56:1093–106.
11. Wei DY et al. Pract Neurol. 2019;19:521–8.