Osteoarthritis
Many chronic conditions are challenging to manage. Here we focus on key pain conditions with a high unmet need among patients and/or healthcare professionals.
Our aim here is to provide the pain community with in-depth information about these conditions; from disease understanding to management approaches.
Osteoarthritis is the most common degenerative joint disease, affecting 25% of the adult population.1 It is characterised by the breakdown of articular cartilage, alterations in subchondral bone (including formation of osteophytes), inflammation within the synovium and synovial fluid, and deterioration of the ligaments and muscles in the affected joint.2 Typically, it primarily affects the joints in the hand, hip and knee, with the knee being the most common area affected.3
Osteoarthritis is a leading cause of disability worldwide, affecting 25% of the adult population, and it is associated with high socio-economic costs.1,8 The peak in osteoarthritis incidence is around 75 years of age and the most common site is the knee, followed by the hand and the hip.3 It is a commonly diagnosed disease in general practice, with the prevalence ever-increasing because of conditions such as obesity, which increase the risk of developing osteoarthritis.3 According to the World Health Organization, by 2050, it is estimated that 130 million people will suffer from osteoarthritis and 40 million will be severely disabled by the disease.8
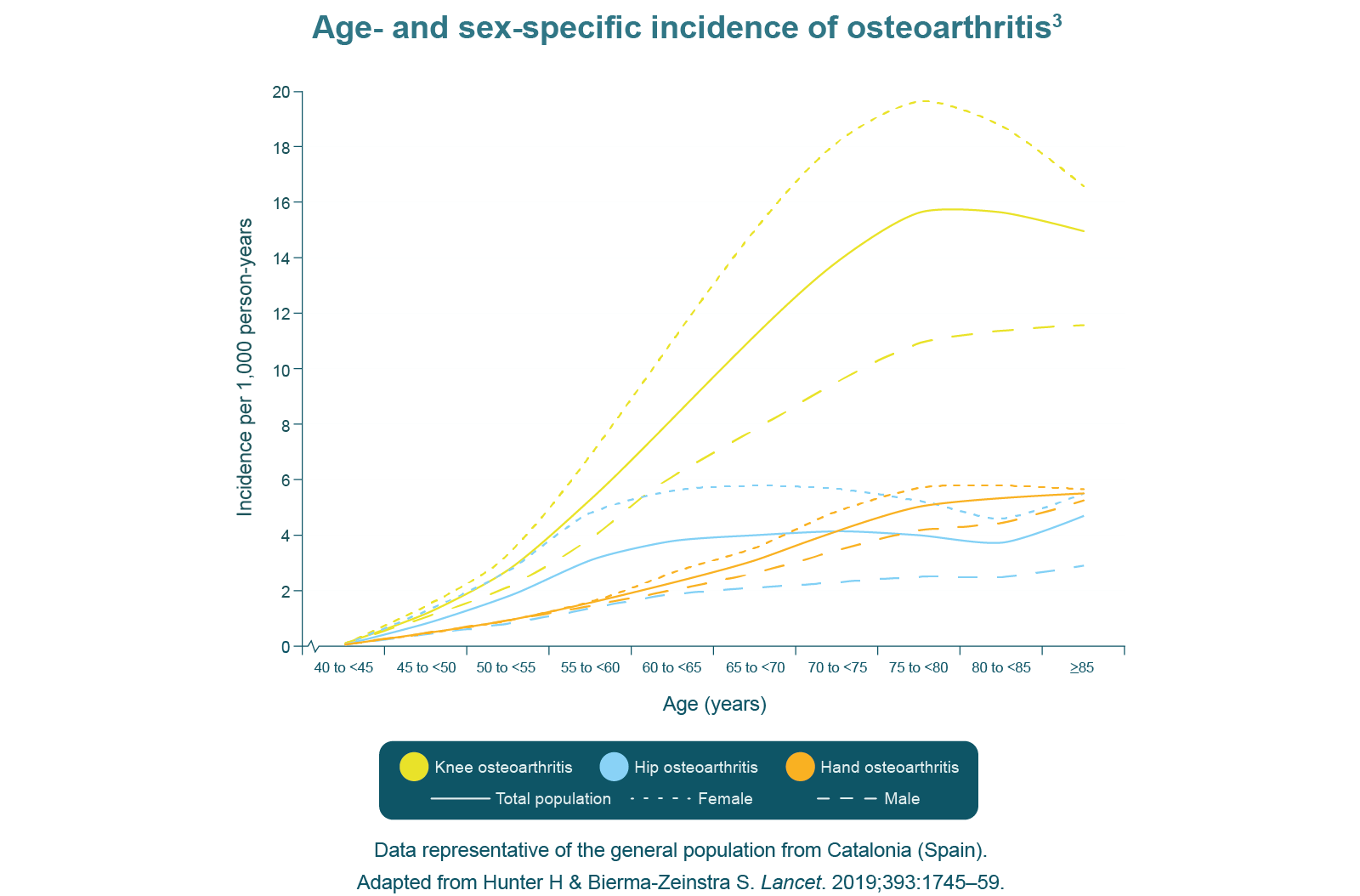
One of the predominant risk factors for osteoarthritis is age, with many people over the age of 65 presenting with radiographic changes in one or more joints.1 Obesity is another risk factor for osteoarthritis as a result of the increased biomechanical loading of joints and low-grade systemic inflammation caused by adipokine secretion.1 Knee injury is the major cause of osteoarthritis in young adults, increasing the risk 4-fold.1 There is also an inherited risk associated with osteoarthritis, which includes over 80 gene mutations or single-nucleotide polymorphisms involved in its pathogenesis.1
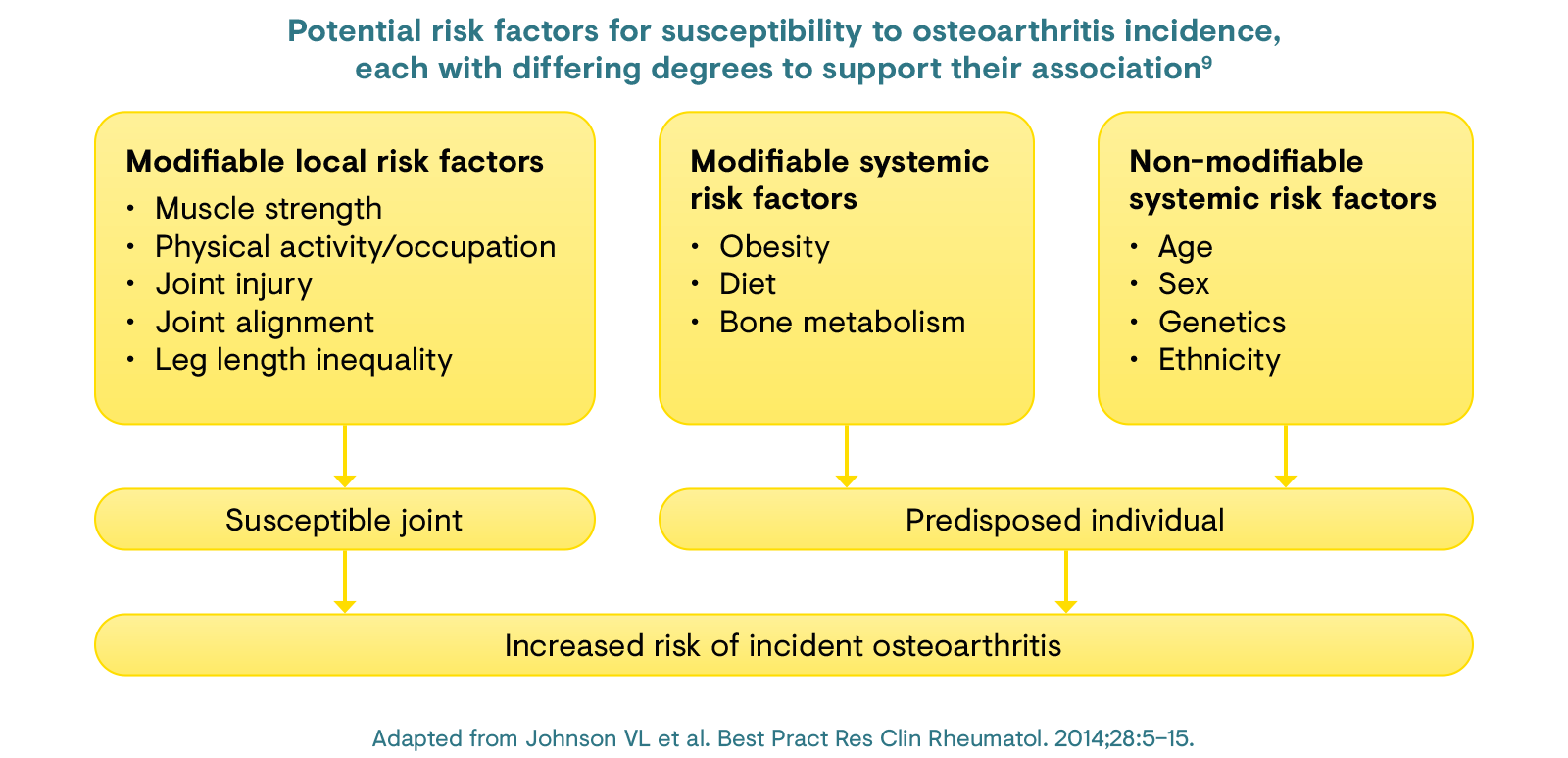
Osteoarthritis is predominantly related to age and its associated processes: cartilage, synovium, and subchondral bone and muscle are affected through ageing and are thought to contribute to changes in joint loading.1 Obesity is the second leading cause of osteoarthritis as a result of the increased joint loading and an increased composition of adipose tissue, which leads to increased secretion of adipokines that contribute to low-grade systemic inflammation.1 Sports injury, particularly knee injury, is the major cause of osteoarthritis in the younger population.1 Cartilage tear, joint dislocation, and ligament strains and tears are the most common injuries that lead to osteoarthritis.1
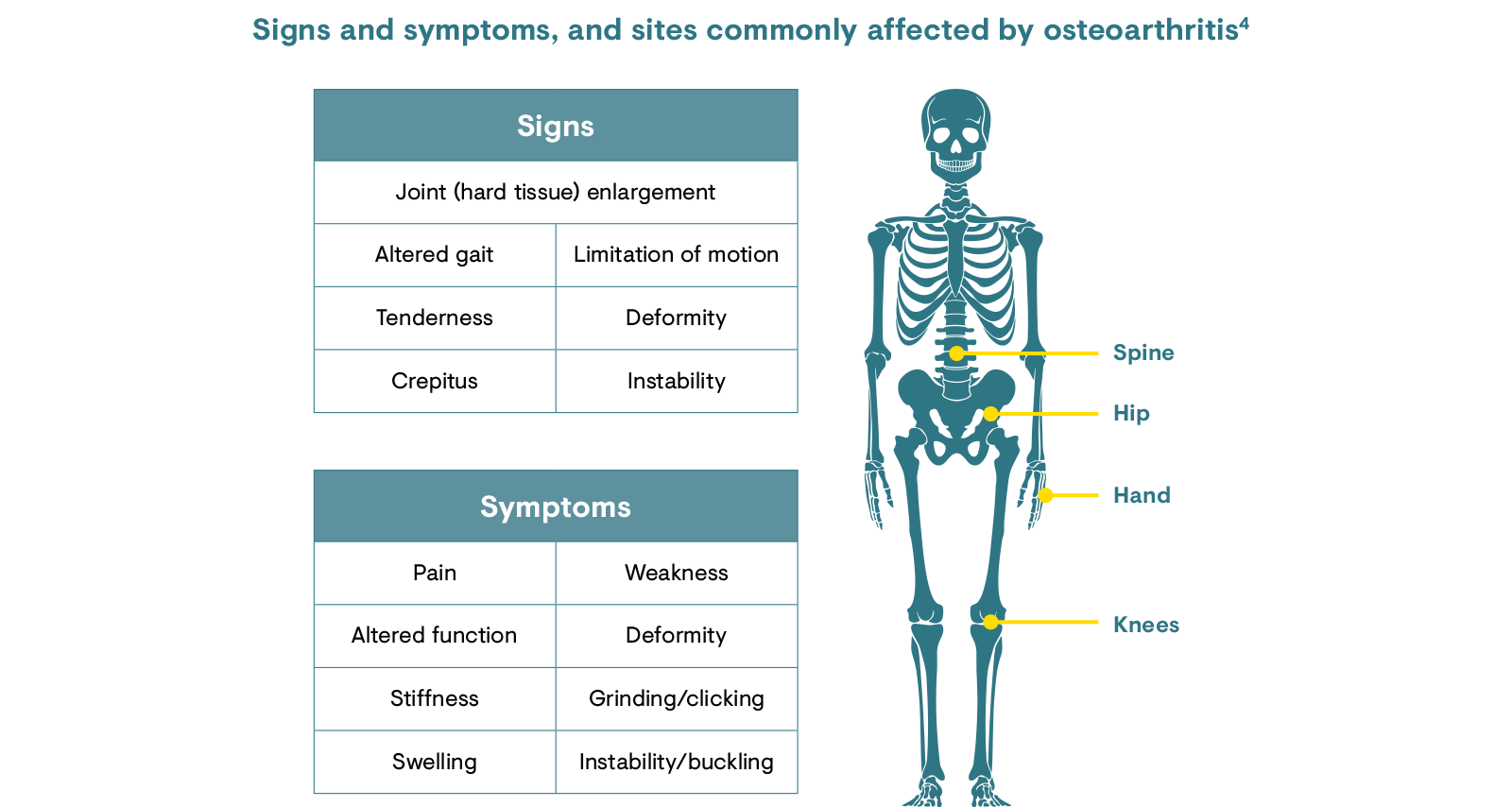
Osteoarthritis is a progressive disease in which symptoms develop and worsen over time. The onset is often insidious, beginning in one or a few joints, with frequent asymmetry of symptoms.4 Signs and symptoms of osteoarthritis include painful joints, stiffness, swelling and instability. The affected area can present as swollen and enlarged.3,4
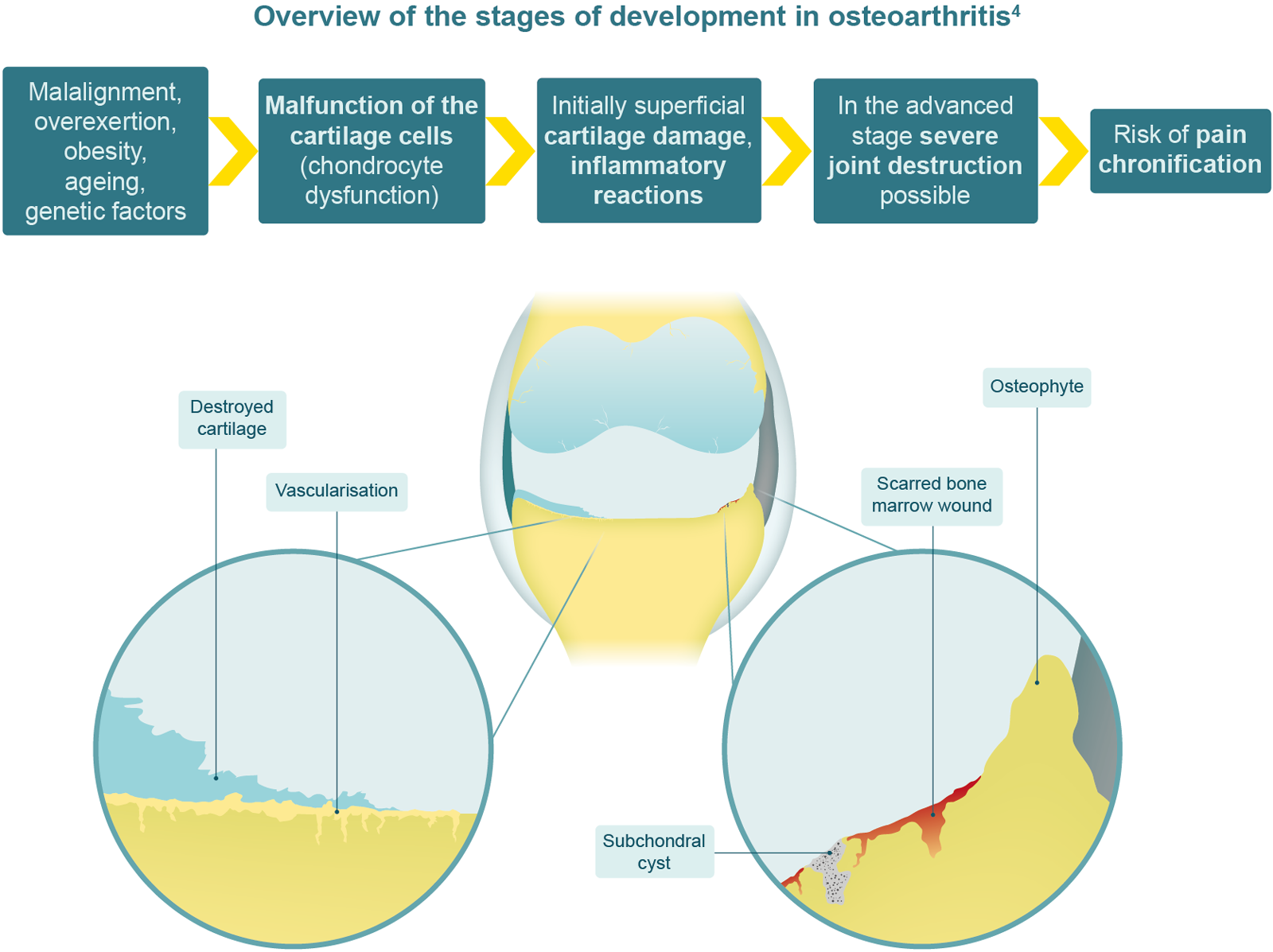
Osteoarthritis was once considered to be a disease of the cartilage, but research has since shown that it does, in fact, involve the whole joint.9 Loss of cartilage precedes a number of cellular changes and the altered biomechanics lead to secondary changes, which include bone remodelling, osteophyte formation, lesions, meniscal tears and extrusion, as well as changes in the synovium, joint capsule, ligaments and periarticular muscles.3
Articular cartilage is composed of extracellular matrix (water, collagen, proteoglycans and calcium salt) and chondrocytes.10 Chondrocytes mediate the turnover of matrix components. In osteoarthritis, chondrocytes fail to maintain the balance between synthesis and degradation of extracellular matrix components.10
A trauma causing a microfracture or inflammation causes release of so-called ‘wear’ particles, which are engulfed by resident macrophages.10 Wear particles stimulate chondrocytes to release degradative enzymes and disrupt the joint homeostasis.10 The breakdown of collagen and proteoglycan stimulates the release of inflammatory cytokines including tumour necrosis factor-α, interleukin (IL)-1 and IL-6, which bind to chondrocyte receptors and stimulate further cartilage degradation.10 The disruption to homeostasis results in increased water and decreased proteoglycan content of the extracellular matrix, and apoptosis of chondrocytes. In time, articular cartilage is destroyed, leaving the underlying bone plate exposed.10
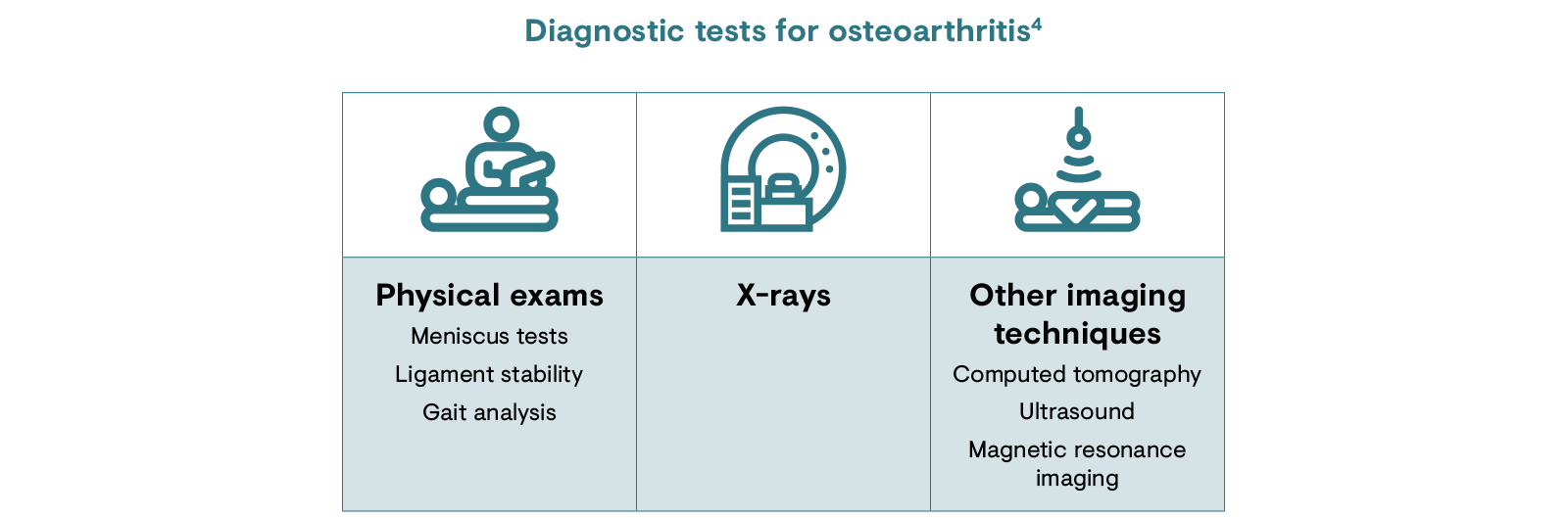
Osteoarthritis should always be suspected in patients who have joint-specific pain (typically usage-related) and loss of function, especially in the elderly.4 The primary goal of a diagnostic evaluation is to demonstrate the presence or absence of osteoarthritis. Physical tests for osteoarthritis include inspection and palpation as well as range of movement and functional tests.4
X-rays are the most commonly used radiological method in diagnosing osteoarthritis, and can be used to highlight cartilage loss and changes in the subchondral bone (e.g. development of bone spurs, sclerosis, cysts and loss of bone volume).4 Other imaging techniques are used to confirm an osteoarthritis diagnosis. Sometimes, fluid from the joint and blood tests will be taken to rule out other conditions.11 It is important to note that there is a discord between structural imaging techniques and pain experienced by the patient, whereby the severity of osteoarthritis described via imaging does not accurately represent the pain felt by the patient and vice versa. In this way, imaging techniques are poor tools for assessing osteoarthritis-related pain.12
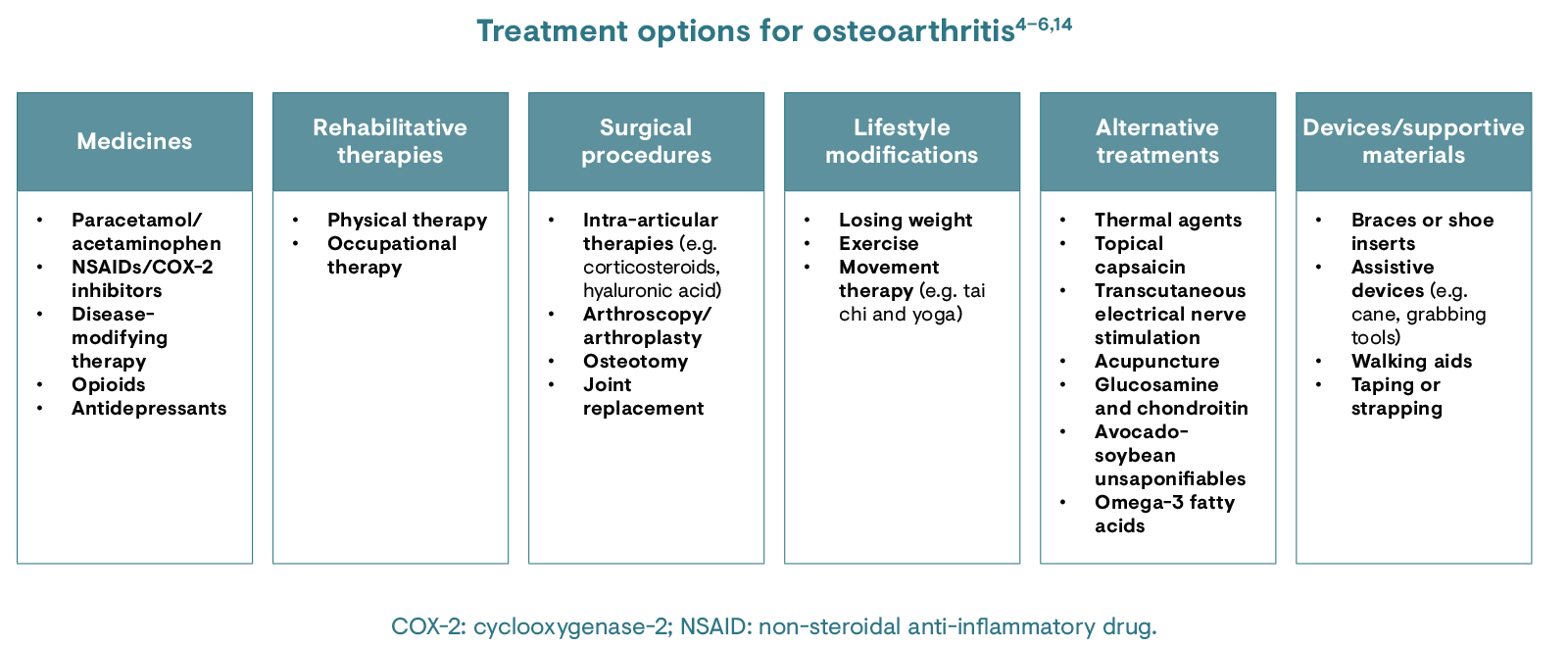
There is no treatment to stop or reverse the effects of osteoarthritis, although there are various methods to reduce pain and increase movement.4 Such management options include paracetamol/acetaminophen and NSAIDs to lessen pain.5,6
Physical therapy is used to strengthen the muscles around the joint and increase flexibility, while occupational therapy may also help patients to perform everyday tasks without pain. For the treatment of more severe osteoarthritis, intra-articular corticosteroid injections may be given.5 Surgery should only be considered in cases where symptoms cannot be adequately managed with more conservative treatment modalities.4 Glucosamine and chondroitin are also alternative treatment options.5,13
Traditionally, pain in osteoarthritis was thought to be purely nociceptive; however, screening tools such as the PainDETECT Questionnaire suggest that a neuropathic component may sometimes be present.15 Psychophysical and neuroimaging data have revealed that some patients with osteoarthritis also experience neuropathic-like pain associated with central sensitisation.15 A trend towards worse outcomes following knee replacement surgery due to osteoarthritis has been observed in this subset of patients with neuropathic‐like pain, when compared with a nociceptive pain group.15
The deeper understanding of the multi-mechanistic nature of osteoarthritis pain has led to the use of centrally acting medicines that may have a benefit of alleviating pain due to osteoarthritis.16 The recognition of subsets of individuals with pain that is refractory to peripherally based treatment, and likely to be centrally mediated, may identify eligible candidates for alternative therapies targeting modulation of central pain pathways.16
There remains a need for alternative approaches to combat pain and inflammation in osteoarthritis. Current treatment approaches focus on managing pain and helping patients find ways to modify their lifestyle to cope with the symptoms of osteoarthritis.17 Pharmacological treatment for osteoarthritis commonly involves the use of NSAIDs or cyclooxygenase-2 inhibitors, which can have negative gastrointestinal and cardiovascular side effects, as well as a negative impact on kidney function.17 Co-prescription with a proton pump inhibitor is therefore recommended to provide potent and long-lasting inhibition of gastric acid secretion and to heal NSAID-associated ulcers, even if NSAIDs are continued.18,19
The use of DMARDs in osteoarthritis is an approach under investigation that is aimed at slowing, halting and reversing disease progression, and even preventing disease development.7 However, there are numerous challenges over target identification and clinical development.4
1. Chen D et al. Bone Res. 2017;5:16044.
2. Loeser RF et al. Arthritis Rheum. 2012;64(6):1697–707.
3. Hunter H & Bierma-Zeinstra S. Lancet. 2019;393:1745–59.
4. Arden N et al. Atlas of Osteoarthritis. Second edition. London: Springer Healthcare; 2018. Available at: https://www.esceo.org/sites/esceo/files/pdf/OA%20ESCEO%20Atlas%20of%20Osteoarthritis%202nd%20Edition%202018.pdf. Accessed August 2021.
5. Zhang W & Doherty M. Br J Sports Med. 2006;40(8):664–9.
6. Hochberg MC et al. Arthritis Care Res. 2012;64:465–74.
7. Hunter DJ et al. Nat Rev Rheumatol. 2011;7:13–22.
8. World Health Organization. Background Paper 6.12. Osteoarthritis. 2013. Available at: https://www.who.int/medicines/areas/priority_medicines/BP6_12Osteo.pdf. Accessed May 2020.
9. Johnson VL et al. Best Pract Res Clin Rheumatol. 2014;28:5–15.
10. Man GS & Mologhianu G. J Med Life. 2014;7(1):37–41.
11. Lespasio MJ et al. Perm J. 2017;21:16–183.
12. Neogi T. Osteoarthritis Cartilage. 2013;21(9):1145–53.
13. Kloppenburg M et al. Ann Rheum Dis. 2019;78(1):16–24.
14. De l’Escalopier N et al. Ann Phys Rehabil Med. 2016;59(3):227–33.
15. Soni A et al. Arthritis Rheum. 2019;71(4):550–60.
16. Dimitroulas T et al. Semin Arthritis Rheum. 2014;44(2):145–54.
17. Laufer S. Rheumatology. 2004;43(Suppl 1):i9–15.
18. National Institute for Health and Care Excellence. Clinical Guideline [CG177]. Osteoarthritis: Care and management. 2014. Available at: http://nice.org.uk/guidance/cg177. Accessed May 2020.
19. Scheiman JM. Arthritis Res Ther. 2013;15(Suppl 3):S5.