Migraine
Many chronic conditions are challenging to manage. Here we focus on key pain conditions with a high unmet need among patients and/or healthcare professionals.
Our aim here is to provide the pain community with in-depth information about these conditions; from disease understanding to management approaches.
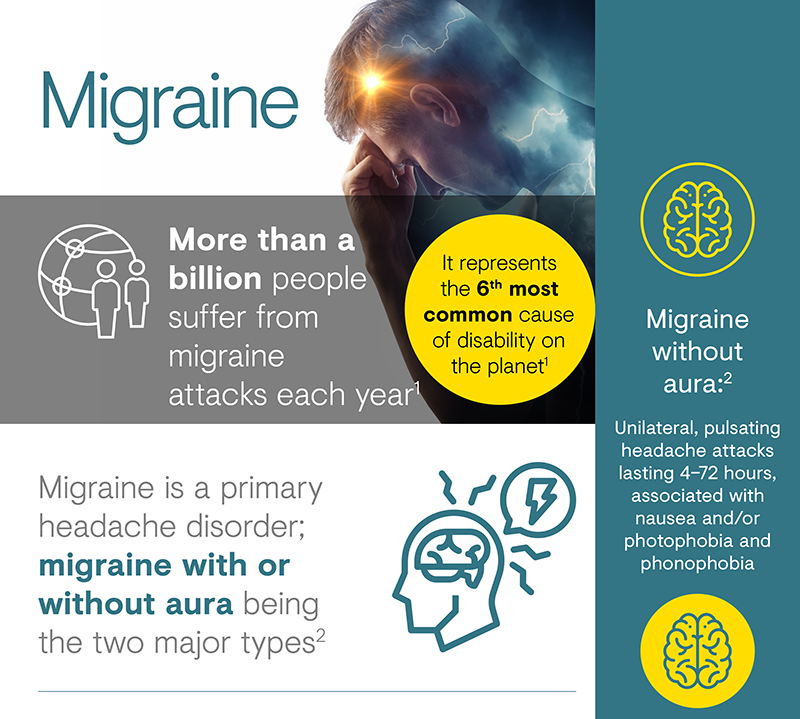
More than a billion people suffer from migraine attacks each year, and it represents the sixth most common cause of disability on the planet.1 A migraine is defined as a unilateral, pulsating headache attack lasting 4–72 hours, accompanied by nausea and/or photophobia and phonophobia.2 Migraine causes significant disability in persons affected and the societal burden is huge, costing €27 billion a year in Europe alone.3
Migraine is the third most common disease in the world, affecting
approximately 1 in 7 people, at a global prevalence of 14.7%.7
It affects 3 times as many women as men, with links to hormonal
differences driving the disease.4,8 Migraine starts at
puberty in many cases but mostly affects people between 35 and 45
years of age; however, it can also present in childhood.9
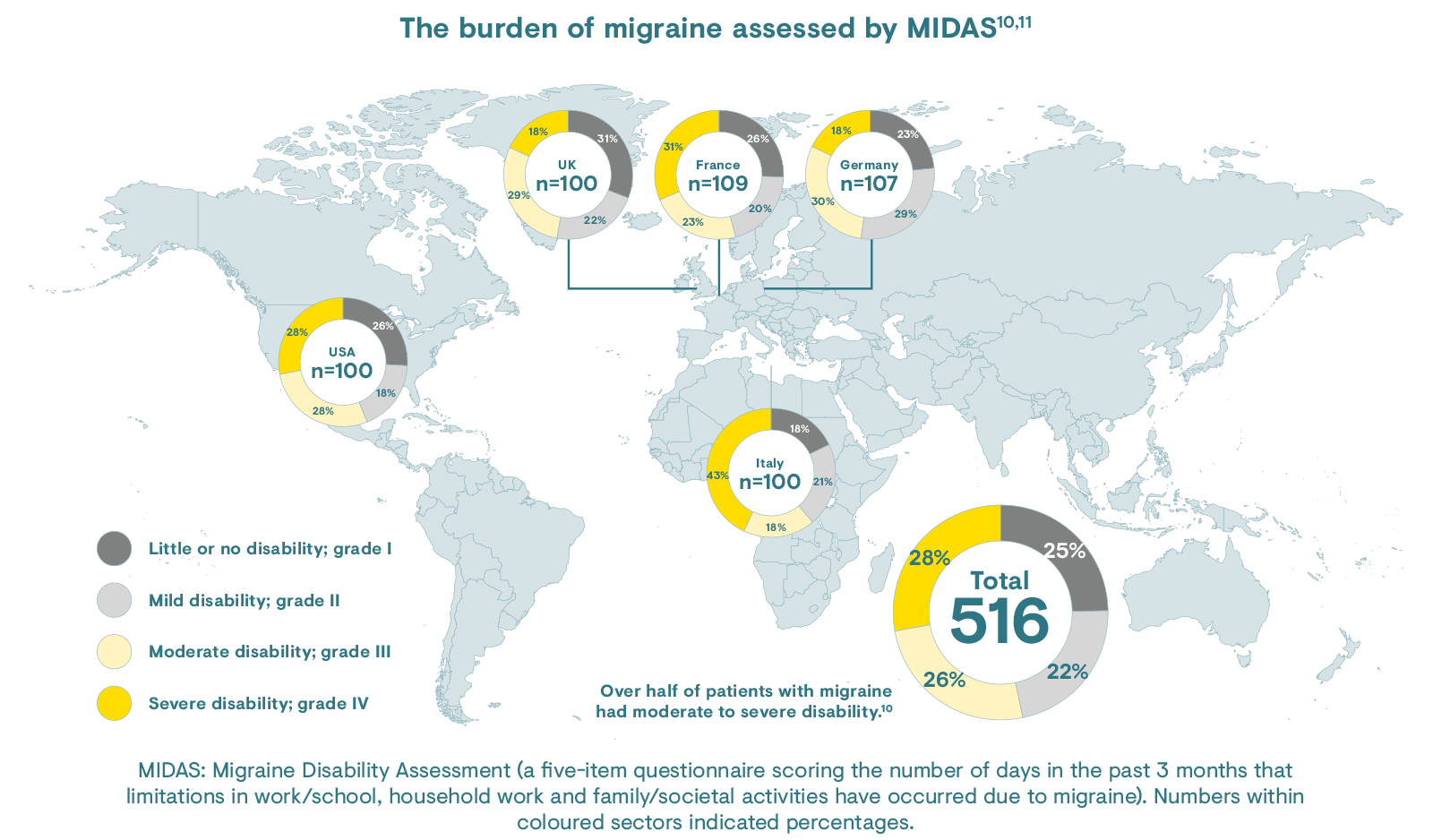
The burden of migraine assessed by Migraine Disability Assessment
(MIDAS) is shown below.10,11 Over half of patients with
migraine had moderate to severe disability.10
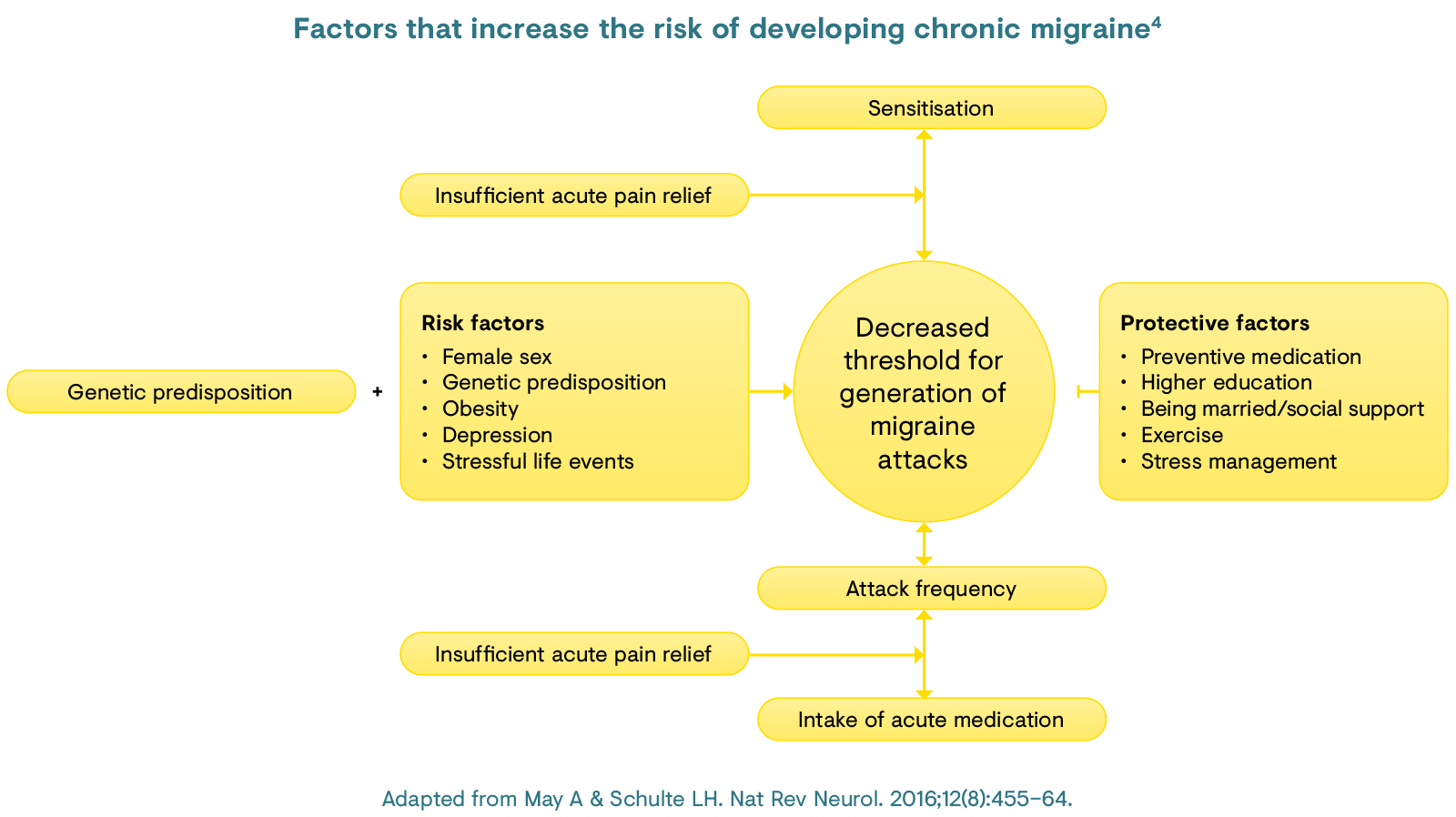
Several risk factors predispose people to chronic migraine, including ineffective or overuse of acute migraine medications, obesity, depression and stressful life events.4 Age, female sex and low educational status also increase the risk of chronic migraine.4 There is also a genetic element to migraine, with mutations in three genes involved in ion transport and neurotransmitter release being implicated in familial hemiplegic migraine.12
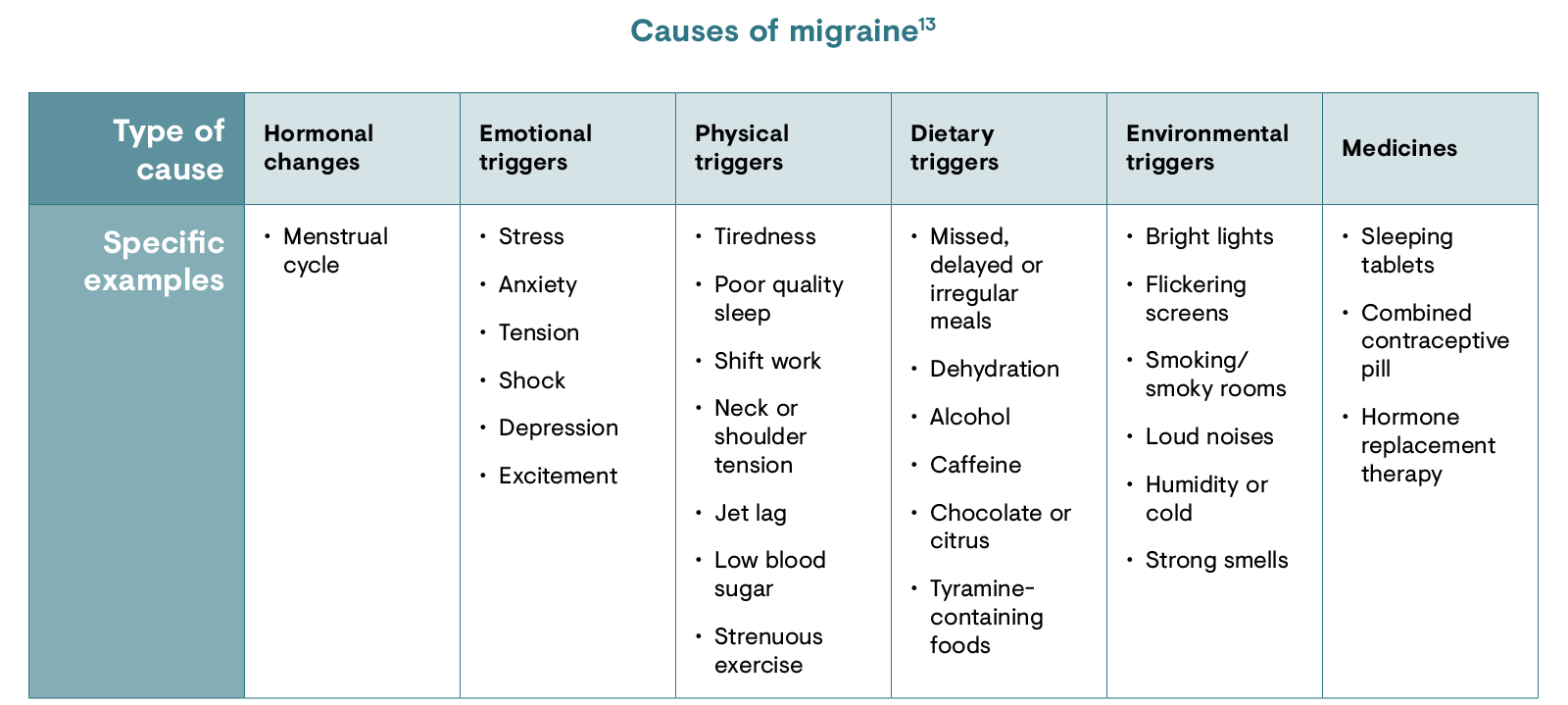
Migraine can be caused by a multitude of factors including ingestion of certain foods, stress, overuse of acute medication, physical activity, low blood sugar, anxiety and shock as well as hormonal changes, sensory stimuli such as bright lights or loud sounds, sleep changes, weather changes and smells.13
Migraine is characterised by headache lasting between 4–72 hours of pulsating quality associated with nausea and/or photophobia and phonophobia.2
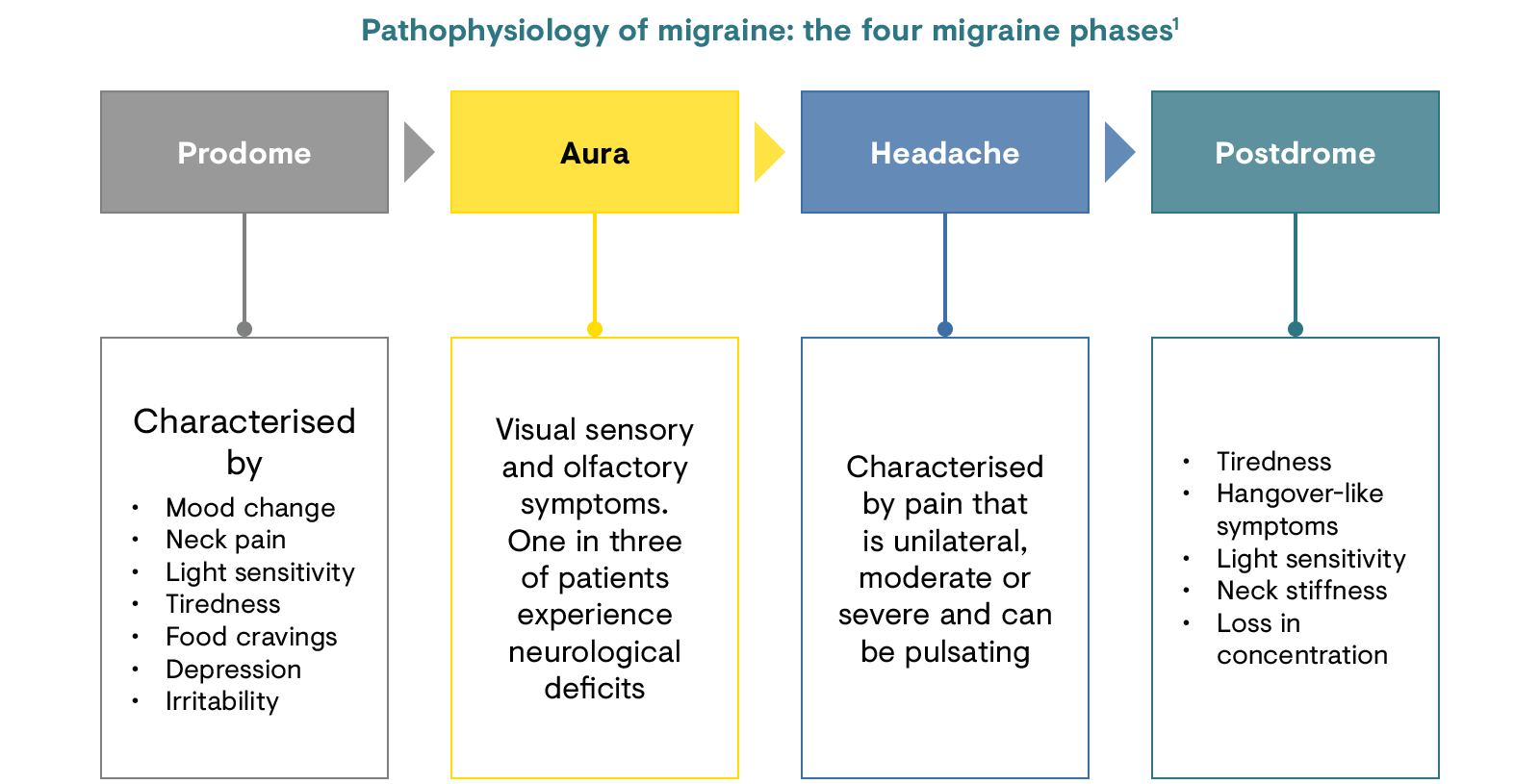
Migraine is split into four characteristic symptom phases: the prodrome/premonitory phase, aura, headache and postdrome.1,14 Not all patients experience all four phases and there are two classifications of migraine based on the presence or absence of the aura phase that precedes the headache.2 Patients who experience the migraine aura also suffer transient focal neurological symptoms.1
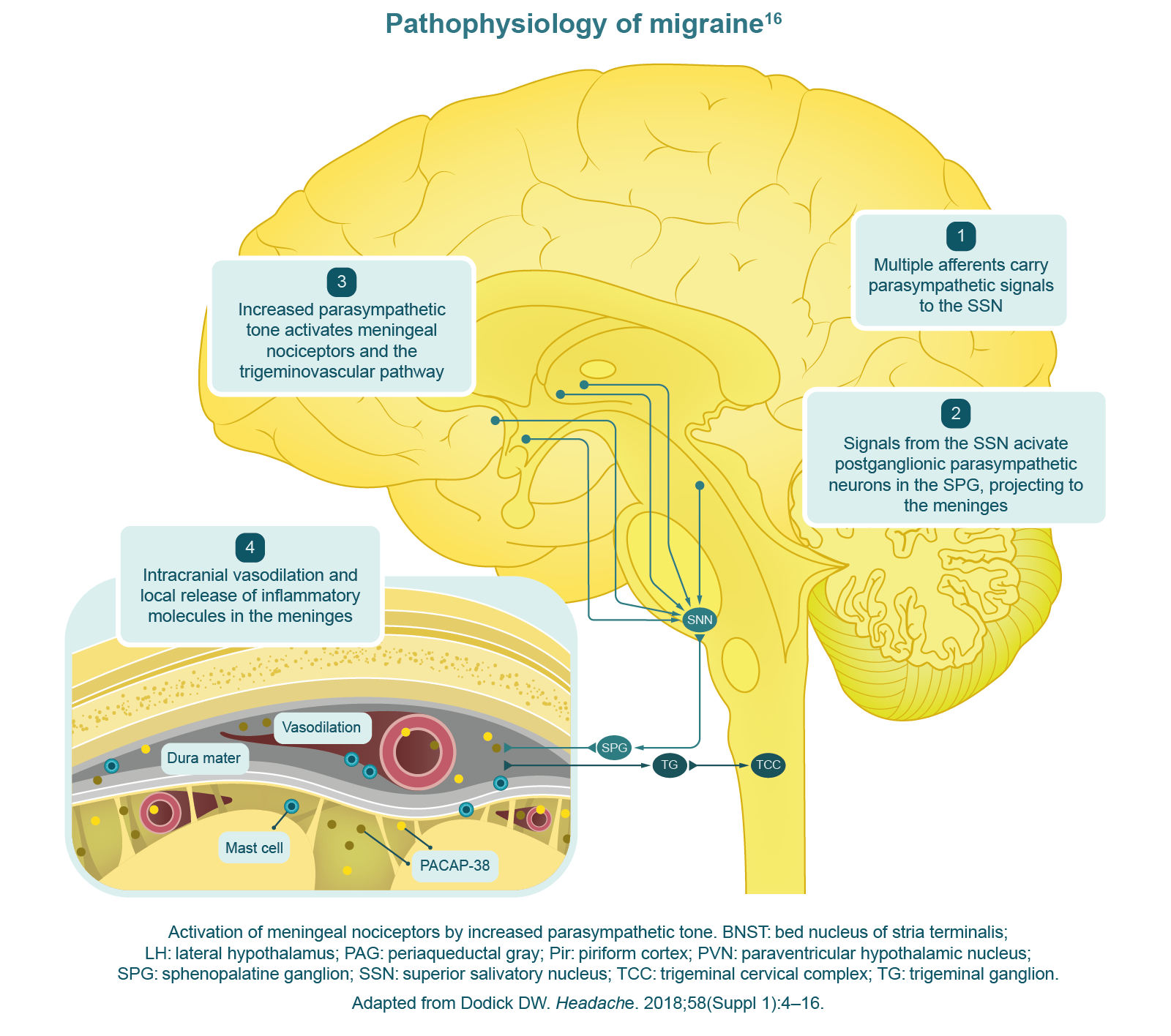
Migraine is a complex brain network disorder involving multiple cortical, subcortical and brainstem regions, which is characterised by neuronal hyperexcitability.15 Nociceptive signals reaching the thalamus are regulated by the release of excitatory and inhibitory neuropeptides/neurotransmitters from hypothalamic and brainstem neurons.16 The inputs from these neurons modulate the allostatic load of the brain, i.e. the amount of stress that can be managed, and determine whether nociceptive signals are relayed to the cortex.15,16
It is argued that increased nociception can also be attributed to a low cyclical brainstem activity, which lowers the threshold for nociceptive signal transmission.15 The hypothalamus is implicated in the prodrome phase, with activations noted in the posterolateral hypothalamus and the midbrain tegmental area, periaqueductal gray, dorsal pons and cortical areas.15
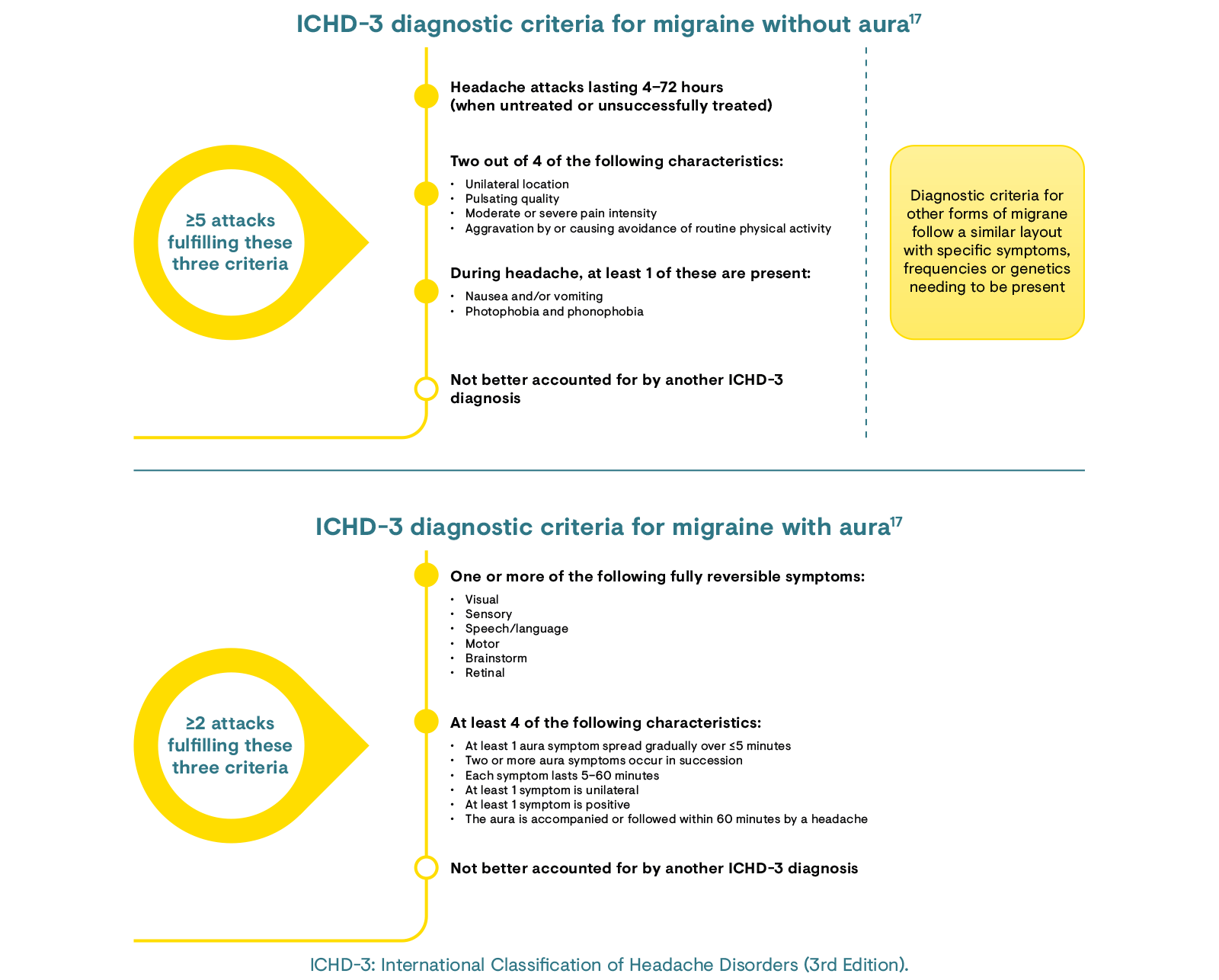
There are two major types of migraine: migraine without aura and migraine with aura, which have slightly different diagnostic criteria as described in the International Classification of Headache Disorders (ICHD).17 There are many subgroups of migraine with aura that are described further in the ICHD-3.17
Acute migraine management includes both non-specific (symptomatic) and specific anti-migraine medications. Predominantly non-specific treatments are used for mild to moderate migraine attacks whereas specific anti-migraine treatments are used in severe cases.18,19 Regular use of acute medication can lead to medication overuse headaches and so care must be taken to avoid this.16
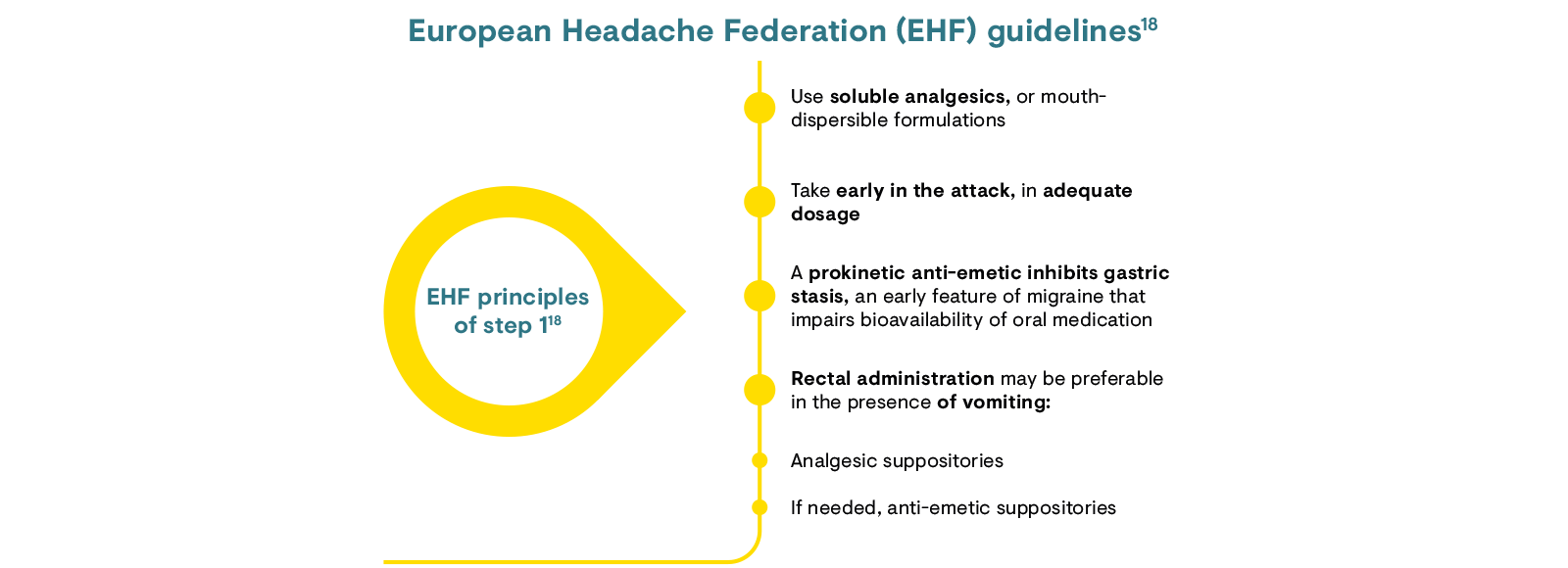
European Headache Federation (EHF) guidelines suggest a stepwise approach to migraine treatment: in step 1, use simple analgesics early on in the attack alongside anti-emetics to avoid gastric symptoms associated with medication; triptans are then used in step 2, when patients do not respond to treatment in step 1.18
The latest International Headache Society (IHS) and EHF guidelines are available here.
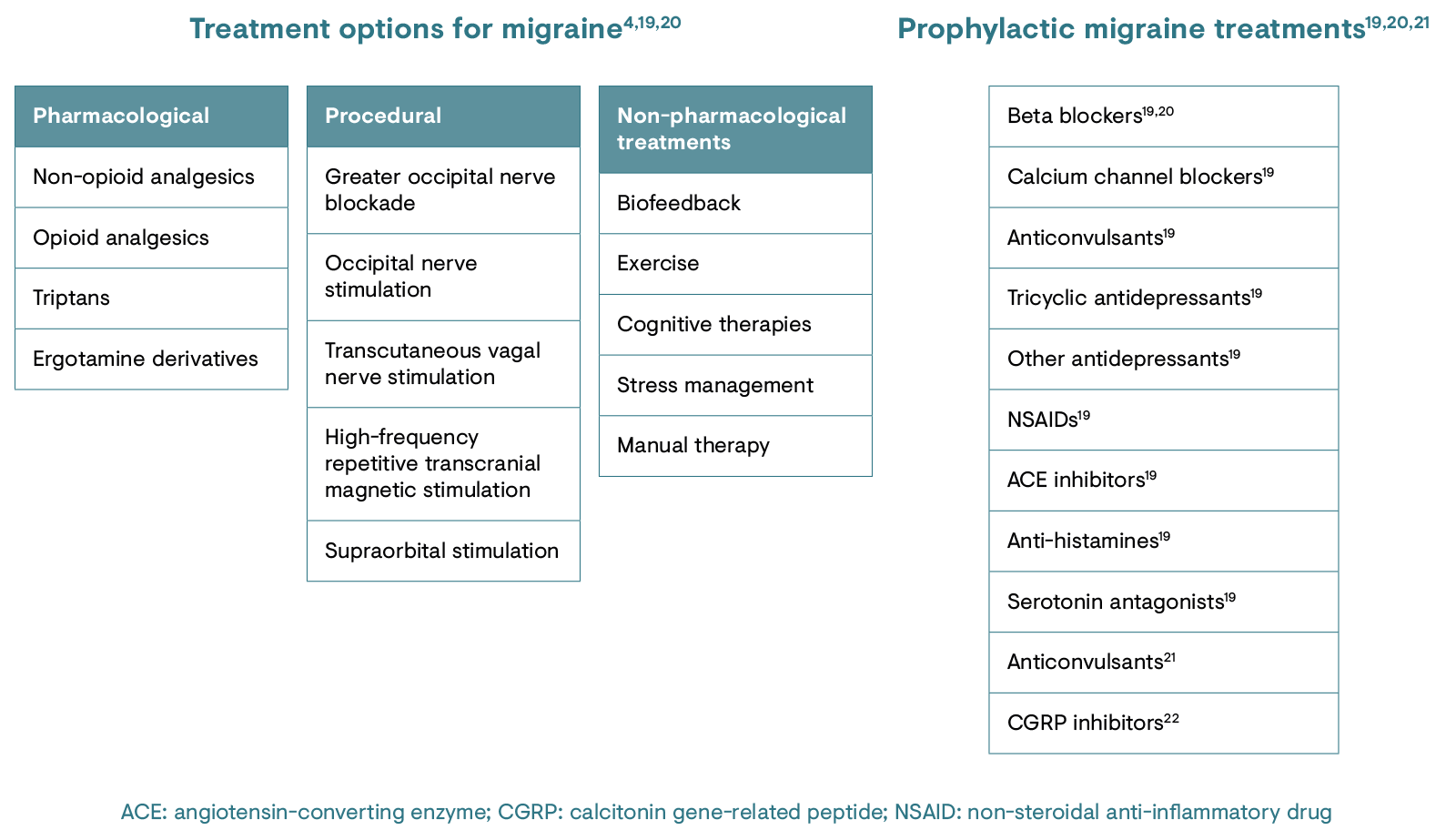
Calcitonin gene-related peptide (CGRP) is involved in pain modulation, perception and sensitisation, and research shows that its activity is increased during migraine attacks.23 Anti-CGRP monoclonal antibodies are a novel option in the prophylactic treatment of migraine.23 Such migraine-specific approaches have the potential to individualise preventive treatment in this condition and improve patient outcomes.23
Current treatments for migraine result only in sustained pain relief for a small subset of patients and can be associated with medication overuse headaches when used frequently.4,6 This is an obvious problem for patients exhibiting frequent migraine episodes. Prophylactic treatments show promise for the prevention of migraine chronification; however, there is a need for specific randomised controlled trials that investigate treatment options for medication overuse headache.4 As well as the need for more detailed studies, education is warranted for patients regarding the dangers of acute medication overuse.6
1. Goadsby PJ et al. Physiol Rev. 2017;97:553–622.
2. National Institute for Health and Care Excellence. British National Formulary. Migraine treatment summary. Available at: https://bnf.nice.org.uk/treatment-summary/migraine.html. Accessed May 2020.
3. European Brain Council. Migraine fact sheet. 2011. Available at: http://ebc-brussels.org/wp-content/uploads/2015/07/Migraine-fact-sheet-Sept-2011.pdf. Accessed May 2020.
4. May A & Schulte LH. Nat Rev Neurol. 2016;12(8):455–64.
5. Steiner TJ & Martelletti P. J Headache Pain. 2007;8(Suppl. 1):S15.
6. Charles A. Lancet Neurol. 2018;17:174–82.
7. Steiner TJ et al. J Headache Pain. 2013;14:1.
8. Misakian AL et al. J Womens Health (Larchmt). 2003;12(10):1027–36.
9. The Migraine Trust. Facts and figures. Available at: https://www.migrainetrust.org/about-migraine/migraine-what-is-it/facts-figures/. Accessed May 2020.
10. MacGregor EA et al. Headache. 2003;43:19–26.
11. Peng KP & Wang SJ. Acta Anaesthesiol Taiwan. 2012;50:69–73.
12. Sutherland HG et al. J Headache Pain. 2019;20(1):72.
13. National Health Service. Migraine causes. 2019. Available at: https://www.nhs.uk/conditions/migraine/causes/. Accessed May 2020.
14. Giffin NJ et al. Neurology. 2016;87(3):309–13.
15. Burstein R et al. J Neurosci. 2015;35(17):6619–29.
16. Dodick DW. Headache. 2018;58(Suppl. 1):4–16.
17. ICHD-3. Cephalalgia. 2018;38(1):1–211.
18. Steiner TJ & Martelletti P. J Headache Pain. 2007;8(Suppl. 1):S2.
19. Antonaci F et al. J Headache Pain. 2010;11:13–9.
20. American Headache Society. Headache. 2019;59(1):1–18.
21. The Migraine Trust. Preventative migraine treatments. Available at: https://www.migrainetrust.org/living-with-migraine/treatments/preventive-medicines/. Accessed May 2020.
22. Deen M et al. J Headache Pain. 2017;18(1):96.
23. Agostoni EC et al. J Headache Pain. 2019;20(1):92.