Pain Basics
Classification of pain
Key points
- Due to the heterogeneity of pain in its duration, anatomical presentation, aetiology, intensity and pathophysiology, there are many ways in which pain can be classified.1
- As pain is complex and multifaceted, it is often necessary to combine different classifications to accurately assess a patient’s pain.1
- A pain classification developed in 2019 by a Task Force of the International Association for the Study of Pain (IASP) recognises the distinction between chronic primary and chronic secondary pain.2
Pain classifications are useful tools in the assessment and diagnosis of patients with pain, and can also guide clinical decision-making when healthcare professionals are ascertaining the most appropriate treatment plan.1
Pain is predominantly defined according to duration (see the ‘Classification according to duration’ section for more information), but may be further classified by anatomical region, aetiology, intensity and pathophysiology. It is often necessary to combine multiple pain classifications to assess a patient’s pain.1 It is important to consider that these different classifications are one-dimensional; to provide optimal care involving a comprehensive assessment and multimodal treatment approach, multiple pain classifications may have to be considered at once.1
References
- Orr PM, et al. Crit Care Nurs Clin N Am. 2017;29:407–18.
- International Association for the Study of Pain (IASP). Chronic pain has arrived in the ICD-11. News bulletin. 2019. Available at: https://www.iasp-pain.org/PublicationsNews/NewsDetail.aspx?ItemNumber=8340&navItemNumber=643. Accessed January 2020.
Classification according to aetiology
Aetiological pain classification aims to delineate the cause of the pain and can be broadly divided into cancer and non-cancer pain.1 Traditionally, chronic pain associated with cancer has been considered as a separate entity due to its complicated aetiology and the more aggressive treatment approaches that are often used.2 However, there is no evidence to suggest that the neural mechanisms underlying cancer pain are distinct from other chronic pain conditions.2 Other causal factors for pain include acute injury, underlying diseases or conditions, and treatment associated with these injuries or conditions, such as surgeries.1
References
- Orr PM et al. Crit Care Nurs Clin N Am. 2017;29:407–18.
- Stanos S et al. Postgrad Med. 2016;128(5):502–15.
Classification according to pathophysiology
Pain can be classified as nociceptive, neuropathic or, in the case of chronic pain only, central sensitisation, depending on the type of injury/insult and the pathophysiological pathway that leads to the perception of pain.1,2
Nociceptive pain describes a normal physiological response to tissue damage resulting from trauma, non-healing injury or inflammatory processes.1,3 The International Association for the Study of Pain (IASP) defines nociceptive pain as “pain that arises from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors”.4 There are two categories of nociceptive pain: somatic pain refers to injuries of the musculoskeletal system and visceral pain refers to internal organ injury and is often felt indirectly.2
Neuropathic pain is defined as pain caused by a lesion or disease of the somatosensory nervous system and occurs as a result of abnormal neural activity.1,2 Neuropathic pain can be described as central or peripheral, depending on whether the lesion is in the peripheral or central nervous system.1
Central sensitisation (also known as nociplastic pain) is defined as pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors, nor evidence for disease of or lesions within the somatosensory system causing the pain.1–3
References
- Clauw DJ et al. Postgrad Med. 2019;131(3):185–98.
- Orr PM et al. Crit Care Nurs Clin N Am. 2017;29:407–18.
- Stanos S et al. Postgrad Med. 2016;128(5):502–15.
- International Association for the Study of Pain (IASP). IASP terminology. 2017. Available at: https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698&navItemNumber=576. Accessed June 2020.
Classification according to anatomical location
Anatomical pain classification is used to determine what part(s) of the body the patient experiences pain.1 It is often the first step during pain assessments.1 Somatic pain is specific to the site of injury and arises from pain receptors activated in bones, muscles, skin, joints, ligaments, tendons and connective tissue.2 In contrast, visceral pain arises in internal organs, but the pain associated with an internal injury is difficult to localise because of the low density of nociceptors in the viscera and the fact that afferent fibres are less well represented in cortical mapping.3 Not considering acute pain conditions, the most common sites of chronic pain are the back and the joints, followed closely by neck- and headache-related pain, according to a European survey.4
References
- Orr PM et al. Crit Care Nurs Clin N Am. 2017;29:407–18.
- Murphy P. Somatic Pain. In: Schmidt R & Willis W (eds). Encyclopedia of Pain. Heidelberg, Germany: Springer; 2007:2190–1.
- Steeds CE. Surgery. 2016;34(2):55–9.
- Breivik H et al. BMC Public Health. 2013;13:1229.
Classification according to intensity
Pain intensity is defined as the magnitude of pain experienced.1 There are various tools that can be used to measure pain intensity, including the visual analogue scale, the verbal rating scale, the numerical rating scale and graphic scales.1,2 These measures require the patient to subjectively measure the magnitude of their pain based on numerical or verbal descriptors.1 There are also measures, such as the Face, Legs, Activity, Cry, Consolability (FLACC) pain scale, that can be used to assess pain in patients that are unable to communicate their pain adequately.3
References
- Cook KF et al. Neurology. 2013;80(Suppl. 3):S49–53.
- Orr PM et al. Crit Care Nurs Clin N Am. 2017;29:407–18.
- Face, Legs, Activity, Cry, Consolability (FLACC) Behavioral Pain Assessment Scale. Available at: https://wps.prenhall.com/wps/media/objects/3103/3178396/tools/flacc.pdf. Accessed June 2020.
Classification according to duration
Pain can be described as acute or chronic, depending on the duration of time that a patient experiences pain.1
Acute pain is short term and resolves within 3–6 months.1 It is the body’s response to a specific injury or trauma and it serves a biological purpose.1 The most important feature of acute pain is that it is self-limiting;2 resolution of pain occurs with tissue healing or repair.1
In some cases, however, acute pain may transition to chronic pain, which is defined as pain that lasts for longer than 3 months, persisting beyond the normal time of healing and that serves no biological purpose.1–3
References
- Orr PM et al. Crit Care Nurs Clin N Am. 2017;29:407–18.
- Grichnik KP & Ferrante FM. Mt Sinai J Med. 1991;58(3):217–20.
- World Health Organization (WHO). International Classification of Diseases 11th Revision (ICD-11). MG30 Chronic pain. 2019. Available at: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1581976053. Accessed June 2020.
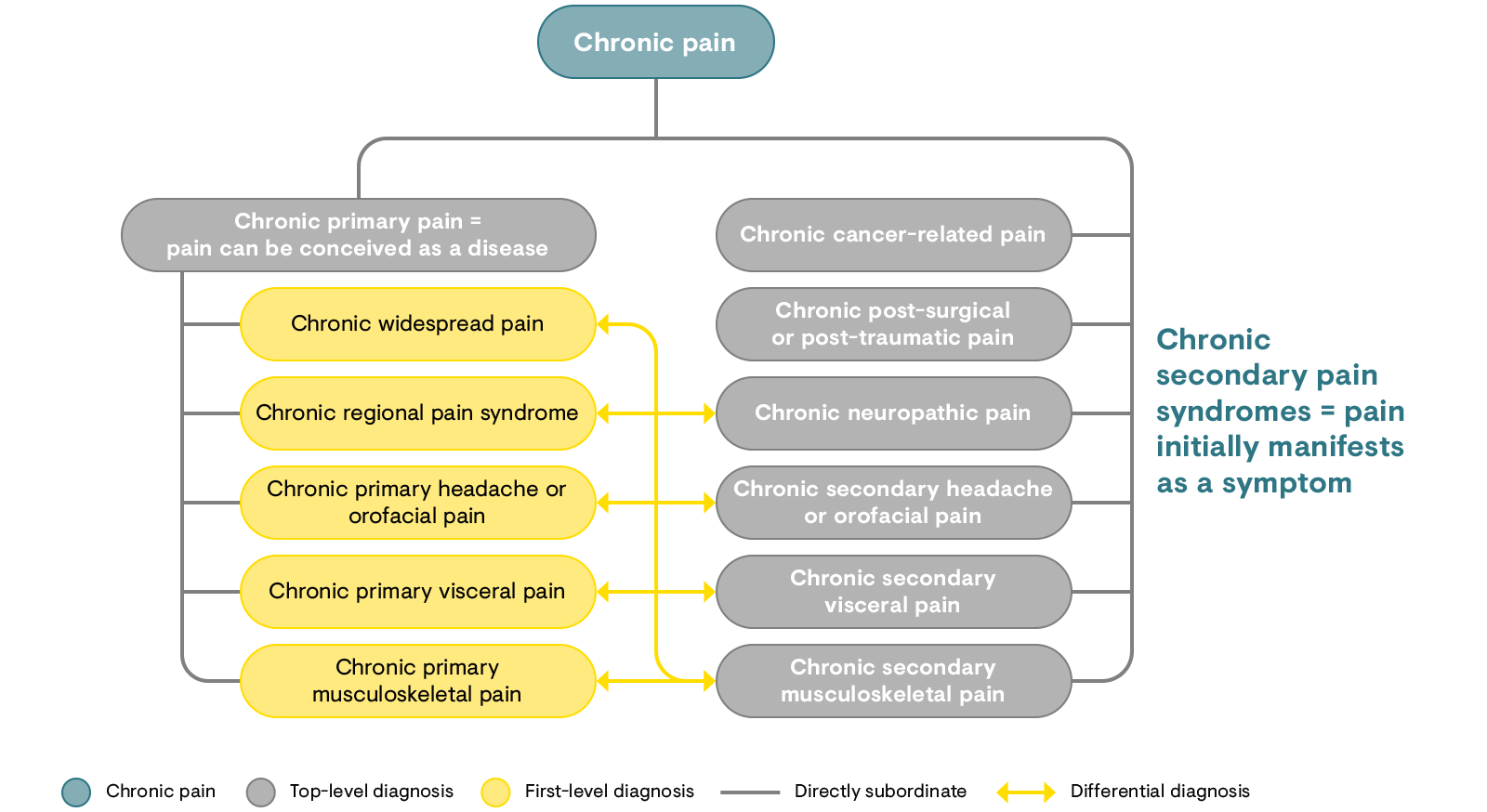
The ICD-11 classification of chronic pain
The 11th revision of the International Classification of Diseases (ICD-11) outlines seven distinct categories for the diagnosis of chronic pain (Figure 1).1 Chronic primary pain (MG30.0) is the first subcategory of chronic pain and refers to persistent pain associated with significant emotional distress or functional disability (i.e. pain can be conceived as a disease in itself).1 In the remaining six subgroups (MG30.1 to MG30.6) pain is secondary to an underlying disease and these are summarised as ‘chronic secondary pain’ where pain may at least initially be conceived as a symptom.1 With the implementation of the ICD-11 chronic pain codes in clinical practice, it is hoped that classification and diagnostic coding of the condition will improve.1
References
- Treede RD et al. Pain. 2019;160:19–27.
Figure 1: Structure of the IASP classification of chronic pain.
In chronic primary pain syndromes (left), pain can be conceived as a disease, whereas in chronic secondary pain syndromes (right), pain initially manifests itself as a symptom of another disease such as breast cancer, a work accident, diabetic neuropathy, chronic inflammatory bowel disease, rheumatoid arthritis, etc. Differential diagnosis between primary and secondary pain conditions may sometimes be challenging (arrows), but in either case, the patient’s pain needs special care when it is moderate or severe. After spontaneous healing or successful management of the underlying disease, chronic pain may sometimes continue and hence the chronic secondary pain diagnoses may remain and continue to guide treatment as well as healthcare statistics.
IASP: International Association for the Study of Pain.
[Adapted from Treede et al. 2019.1]
References
- Treede RD, et al. Pain. 2019;160:19–27.