Pain Basics
Management of chronic pain
Key points
- The modern management of chronic pain favours a practical biopsychosocial approach, which considers neurobiology and psychosocial risk factors and encompasses a wide range of pharmacological and non-pharmacological treatment options, rather than a biomedical approach purely focused on pathophysiology.1
- There is a need for good communication within an interdisciplinary team to best address patient needs and manage their pain effectively.2
- Due to the multi-mechanistic nature of chronic pain, a multimodal treatment plan combining therapies with different modes of action can improve patient outcomes.3
According to the UK’s National Institute for Health and Care Excellence (NICE), the focus of treatment for chronic pain should be to reduce a person’s pain with the objective of improving their quality of life.4 Pain treatment can follow a multimodal approach using both pharmacological and non-pharmacological agents in a dynamic fashion and taking into consideration the following:5
- Intensity of the pain
- Pathophysiology of the pain
- Complexity of the symptoms
- Presence of comorbidity
- Social context
- Time of the illness
References
- Clauw DJ et al. Postgrad Med. 2019;131(3):185–98.
- Varrassi G et al. Curr Med Res Opin. 2010;26:1231–45.
- Pergolizzi J et al. Curr Med Res Opin. 2013;29(9):1127–35.
- National Institute for Health and Care Excellence (NICE). Key therapeutic topic [KTT21] Medicines optimisation in chronic pain. Updated September 2019. Available at: https://www.nice.org.uk/advice/ktt21. Accessed June 2020.
- Cuomo A et al. J Pain Res. 2019;12:711–14.
Implementing a practical biopsychosocial approach
A practical biopsychosocial approach may be utilised to manage chronic pain, which encompasses a wide range of pharmacological and non-pharmacological therapies, in addition to teaching self-management techniques and psychological/rehabilitative support.1 Adopting such a model may lead to a more multimodal and multidisciplinary approach to chronic pain management, incorporating a range of treatment strategies that are aimed at reducing pain, minimising disability and improving patient quality of life.1
Reference
- Clauw DJ et al. Postgrad Med. 2019;131(3):185–98.
Multimodal therapy
Pain is often multi-mechanistic and therefore its management requires a multimodal approach where combinations of pharmacological treatments with different mechanisms of actions as well as non-pharmacological approaches are used to provide analgesia.1 This is particularly apparent in cases where both nociceptive and neuropathic components are at play, which respond differently to different types of analgesics or therapies (including non-pharmacological strategies such as physiotherapy, psychotherapy and rehabilitation techniques).1
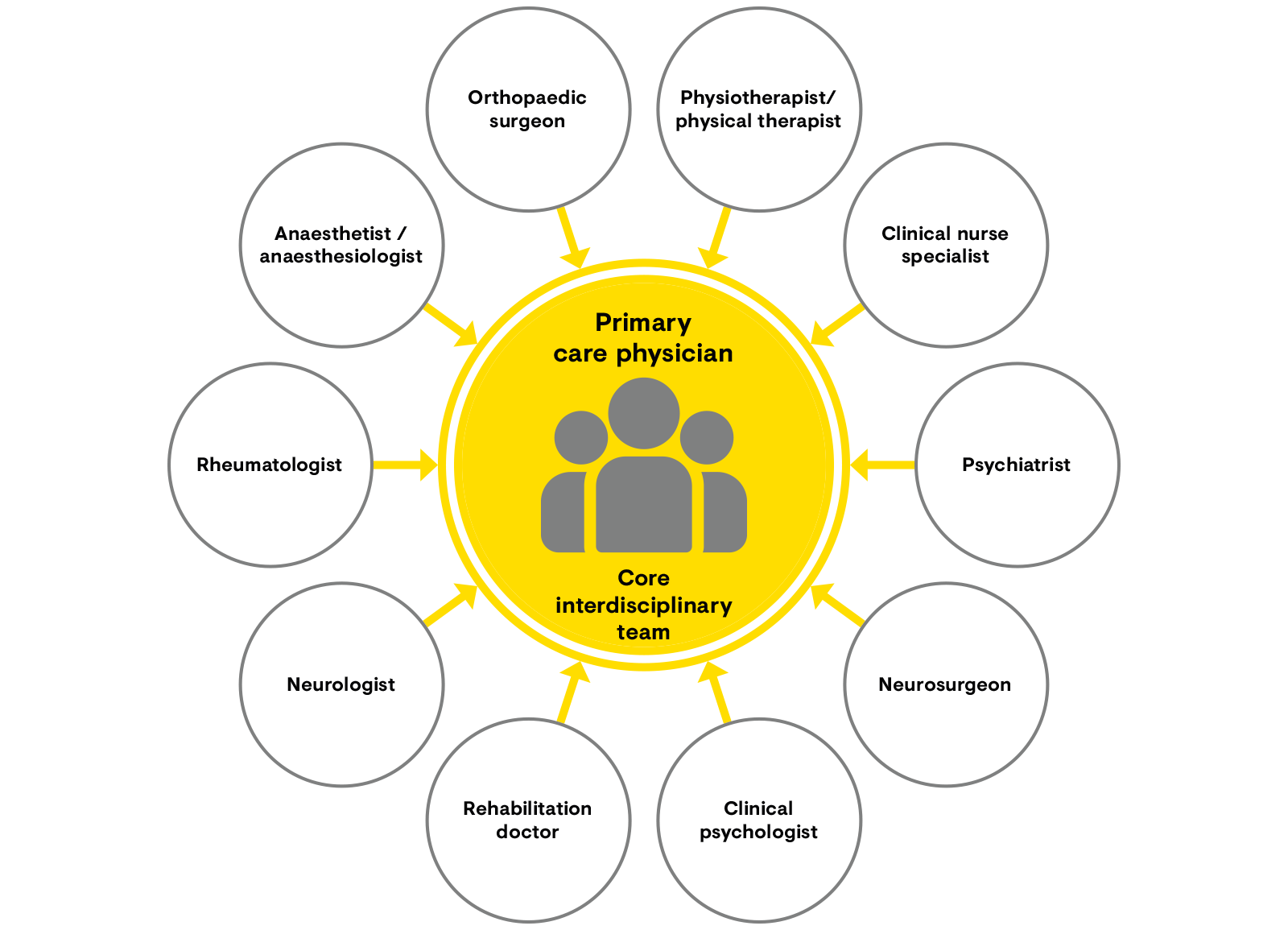
Interdisciplinary management of chronic pain requires a core interdisciplinary team of healthcare professionals.2 The primary care physician acts as gatekeeper and coordinator and has a central role in the long-term management strategy and refers the patient for further treatment as necessary.2 Communication among the team, and between the team and the primary care physician, is extremely important. The interdisciplinary team usually includes a primary care physician, anaesthesiologist, rheumatologist, neurologist and a psychiatrist or psychologist (Figure 1).2 Nevertheless, other specialists may also be included based on the individual patient’s needs. In order to improve outcomes for patients, multimodal therapy delivered by an interdisciplinary team should be considered.
Figure 1: The core multidisciplinary team for the management of chronic pain2
[Adapted from Pergolizzi et al. 2013.2]
References
- Varrassi G et al. Curr Med Res Opin. 2010;26:1231–45.
- Pergolizzi J et al. Curr Med Res Opin. 2013;29(9):1127–35.
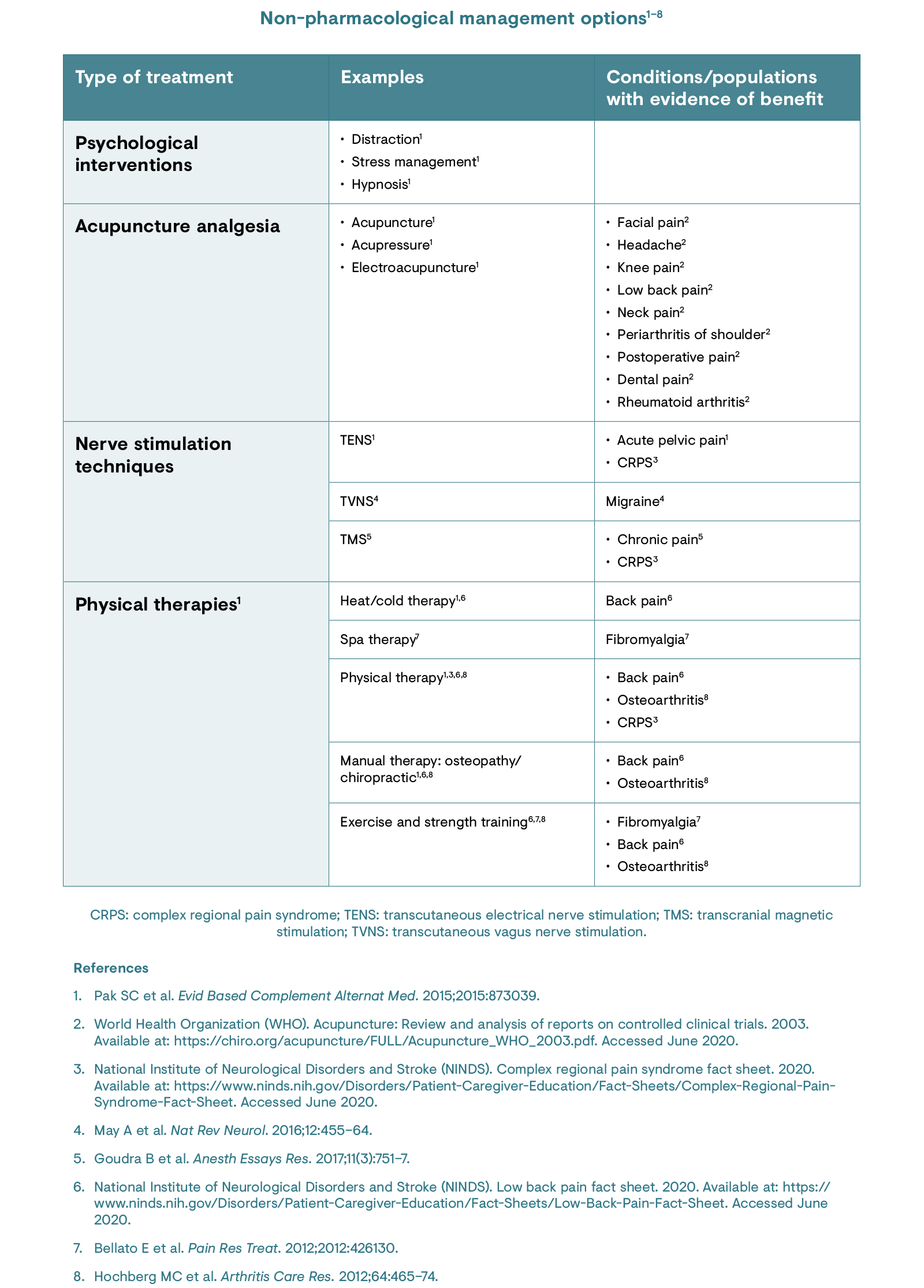
Non-pharmacological management
Non-pharmacological interventions for pain management primarily focus on alleviating pain and can complement or substitute pharmacological therapy.1 Such non-pharmacological interventions may involve activation of anti-nociceptive outputs with an aim to inhibit nociceptive input, strengthening the body’s own pain control mechanisms.1 Non-pharmacological treatment options can be organised into four categories, as follows:1
- Psychological interventions including distraction, stress management, hypnosis and cognitive behavioural interventions
- Acupuncture and acupressure
- Physical therapies including massage, heat/cold therapy, physiotherapy, osteopathy and chiropractic
- Transcutaneous electrical nerve stimulation (TENS).
References
- Pak SC et al. Evid Based Complement Alternat Med. 2015;2015:873039.
Pharmacological treatments
The multifactorial nature of chronic pain requires that effective pain management needs to take into account the underlying pain mechanisms in order to choose targeted treatment.1 Pharmacological treatments should seek to complement – not replace – non-pharmacological therapies.1 This is of particular importance in conditions with a neuropathic component, as presence of this is associated with increased pain severity and duration due to sensitisation.1
In 2019, the World Health Organization (WHO) released updated guidelines for the pharmacological and radiotherapeutic management of pain in cancer.2 Within these guidelines, the importance of careful pain assessment plus differential diagnosis of the type of pain and its site of origin are emphasised.2 It should be noted that these are guidelines only for pain caused by the direct effect of cancer, and many factors should be considered when providing care, using a person-centred and integrated approach.2
There are various options available for the treatment of chronic pain; these can be classified as follows: non-opioids and co-analgesics (adjuvants), topical analgesics, opioids and atypical opioids.
References
- Varrassi G et al. Curr Med Res Opin. 2010;26:1231–45.
- World Health Organization (WHO). WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. January 2019. Available at: https://www.who.int/ncds/management/palliative-care/cancer-pain-guidelines/en/. Accessed June 2020.
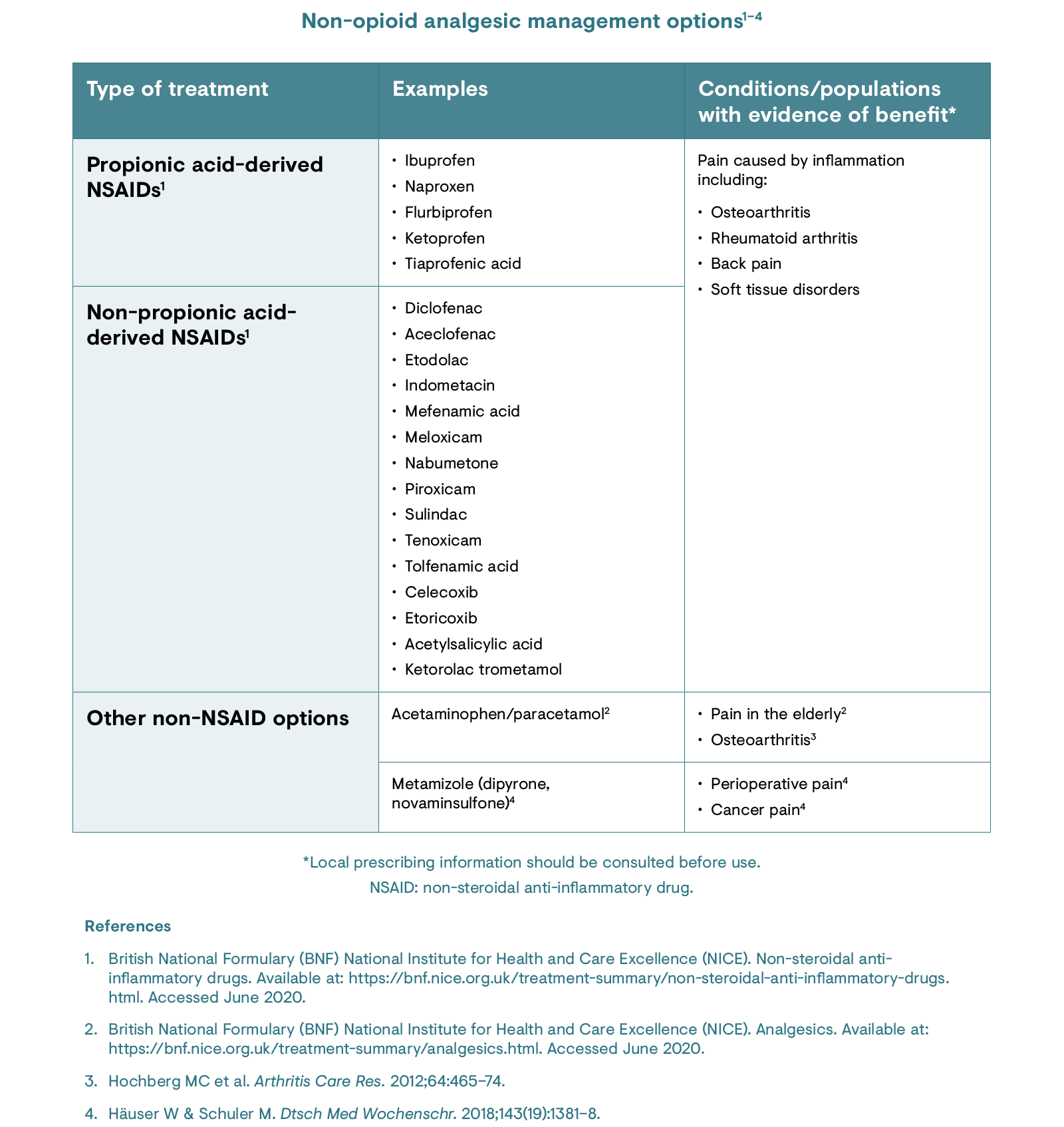
Non-opioid analgesics
Non-opioid drugs include paracetamol/acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs).1,2 Paracetamol/acetaminophen is often preferred in the elderly although caution should be taken with regard to liver toxicity.1 NSAIDs have lasting analgesic and anti-inflammatory effects across a range of chronic pain conditions.2 However, care should be taken with regard to the possibility of cardiovascular and gastrointestinal adverse events, and additional considerations should be taken in elderly populations and with concurrent alcohol consumption.2
References
- British National Formulary (BNF) National Institute for Health and Care Excellence (NICE). Analgesics. Available at: https://bnf.nice.org.uk/treatment-summary/analgesics.html. Accessed June 2020.
- British National Formulary (BNF) National Institute for Health and Care Excellence (NICE). Non-steroidal anti-inflammatory drugs. Available at: https://bnf.nice.org.uk/treatment-summary/non-steroidal-anti-inflammatory-drugs.html. Accessed June 2020.
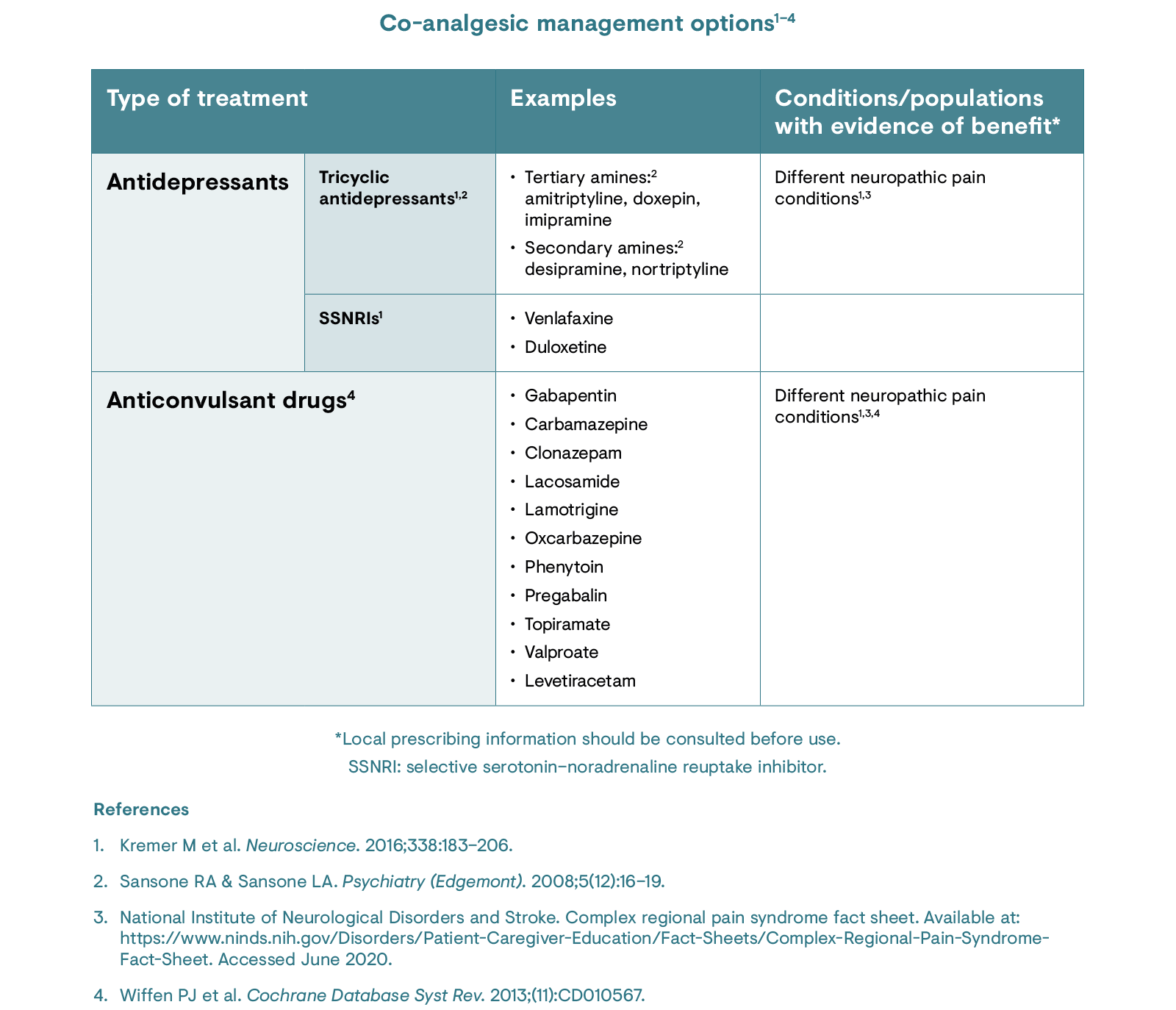
Co-analgesics (adjuvants)
Other non-opioid drugs can be described as co-analgesic/adjuvant medications – therapeutics that were developed for an alternative purpose but have been found to provide analgesic properties.1 The primary groups of co-analgesics are antidepressants and anticonvulsants.1 While many antidepressants are effective in managing pain, they can be associated with a range of side effects, including weight gain, sexual dysfunction, cardiovascular effects, and lethality in overdose.2 Similarly, anticonvulsants have been shown to improve quality of life and function in pain patients, but may lead to adverse events, particularly those associated with the central nervous system (e.g. dizziness, somnolence, gait or balance disturbance, and tremor).3
References
- Center for Substance Abuse Treatment. Managing chronic pain in adults with or in recovery from substance use disorders. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2012. Available at: https://www.ncbi.nlm.nih.gov/books/NBK92048. Accessed June 2020.
- Sansone RA & Sansone LA. Psychiatry (Edgemont). 2008;5(12):16–19.
- Wiffen PJ et al. Cochrane Database Syst Rev. 2013;(11):CD010567.
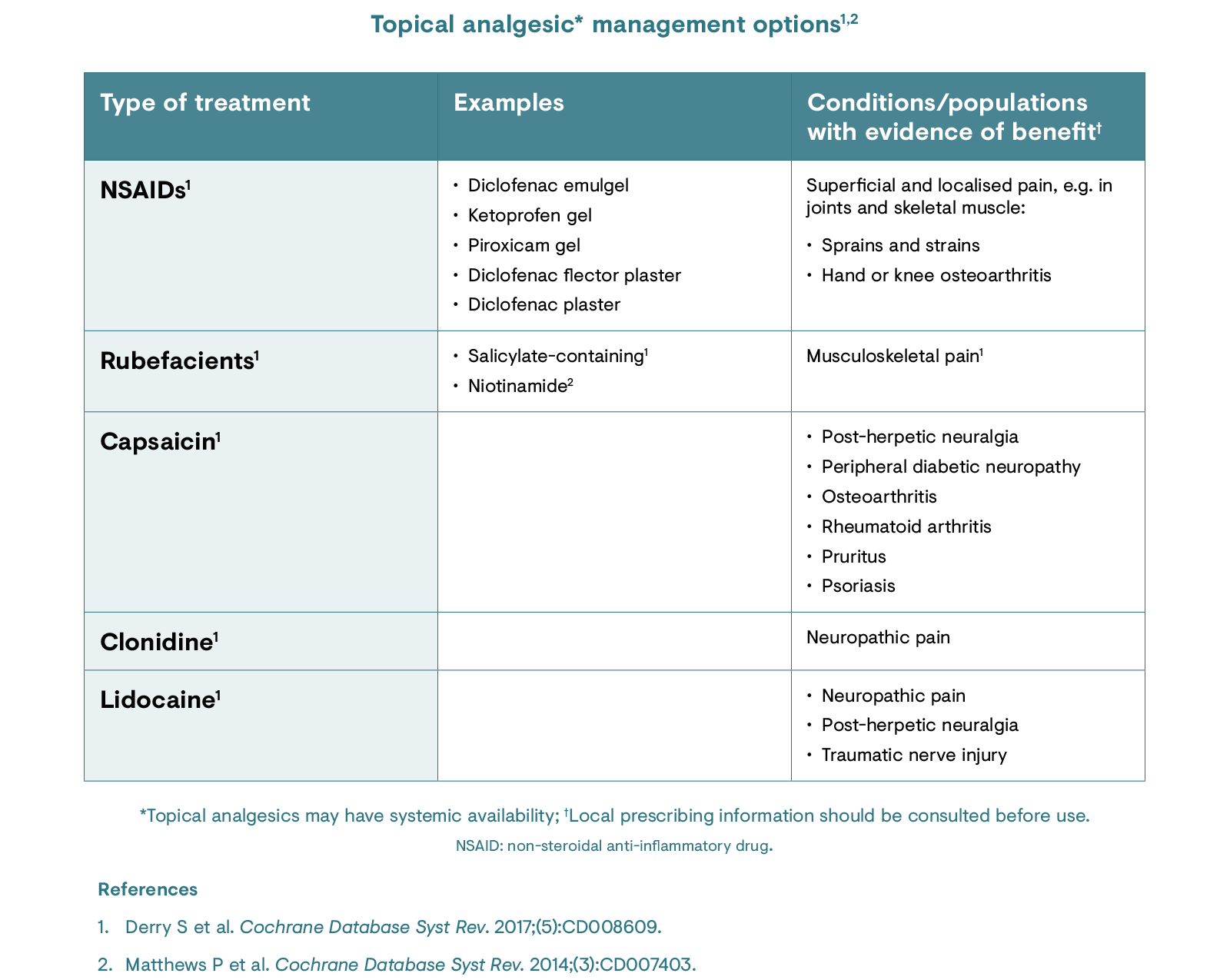
Topical analgesics
Topical analgesics can be applied directly to the skin at specific areas of pain.1 The group of topical analgesics comprises very different mechanisms of action and can therefore not be described as one entity apart from the mode of application being topical. Topical non-steroidal anti-inflammatory drug (NSAID) analgesics inhibit cyclo-oxygenase enzymes, limiting the production of prostaglandins; for more information on NSAIDs, please see the non-opioid analgesics section.1 Rubefacients cause irritation of the skin, which is believed to relieve musculoskeletal pain.1 Other types of topical analgesics can bind to nociceptors in the skin and after repeated application, this can lead to ‘defunctionalisation’, which can reduce pain in the area.1 Topical analgesics are less invasive than other treatments and their administration may limit systemic adverse events by minimising systemic concentrations of the drug.1 However, local side effects including irritation, itching and rash may occur with topical analgesics.1
References
- Derry S et al. Cochrane Database Syst Rev. 2017;(5):CD008609.
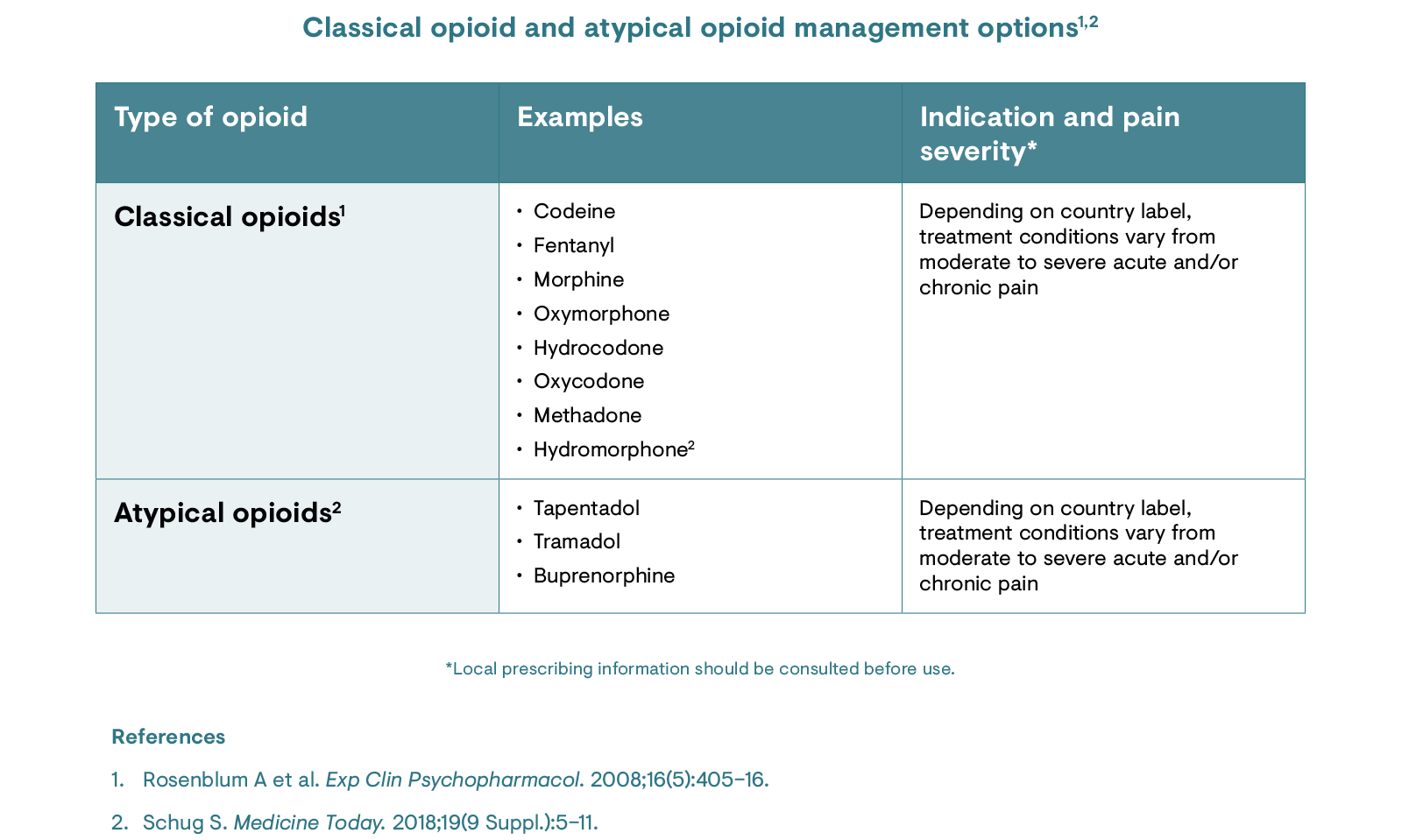
Opioids and atypical opioids
Opioids can be divided into classical or atypical opioids. Classical opioids are compounds that bind to opioid receptors, which are responsible for modulating pain in the central and peripheral nervous system.1 Atypical opioids are analgesics that utilise both opioid and non-opioid mechanisms of action, possibly in a synergistic manner.2
Classical opioids and atypical opioids may be considered if pain remains poorly controlled following non-opioid approaches and if the risk–benefit ratio is favourable.1 They should only be used in carefully selected patients, with risk factors for abuse and addiction reviewed prior to initiation.3 Where opioids are deemed necessary, they should be used at the lowest dose and shortest duration possible, with well-defined treatment goals and continuous evaluation.1,3 Regular monitoring and follow-up should be implemented to ensure that opioids are used appropriately and in alignment with treatment goals (pain intensity and functionality) as agreed with the patient.4,5 Dose adjustments may be made to find the right dose for each individual and gradual downtitration should be considered and tailored to each patient.3 Risk reduction, in terms of abuse, dependence and overdose, is key in cases where long-term opioid use is warranted.1
References
- Clauw DJ et al. Postgrad Med. 2019;131(3):185–98.
- Raffa RB et al. J Clin Pharm Ther. 2014;39(6):577–83.
- British National Formulary (BNF) National Institute for Health and Care Excellence (NICE). Pain, chronic. Available at: https://bnf.nice.org.uk/treatment-summary/pain-chronic.html. Accessed June 2020.
- Faculty of Pain Medicine. Opioids Aware. Available at: https://www.rcoa.ac.uk/faculty-of-pain-medicine/opioids-aware. Accessed June 2020.
- Korsten TR & George TP. Sci Pract Perspect. 2002;1:13–20.
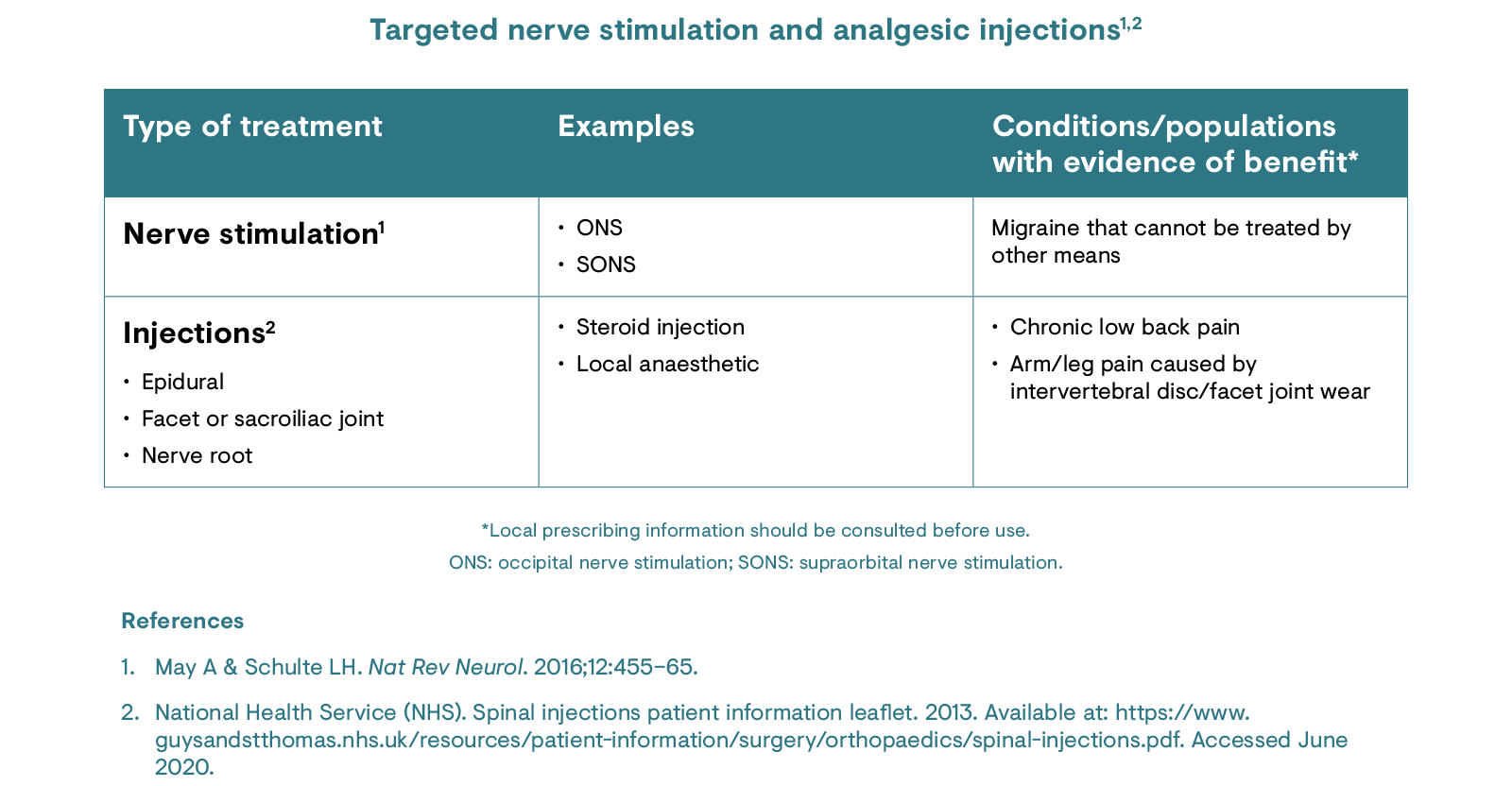
Targeted nerve stimulation and analgesic injections
These modalities may include a more targeted, invasive nerve stimulation such as occipital nerve stimulation, which involves implantation of a device and direct targeting of the occipital nerve.1 Other options include nerve blockades/targeted anaesthetic or steroid injections.2 These management approaches can be invasive and may require anaesthesia (which carries its own risks) and they can lead to severe long-term complications such as infection and skin erosion.1,2
References
- May A & Schulte LH. Nat Rev Neurol. 2016;12:455–65.
- National Health Service (NHS). Spinal injections patient information leaflet. 2013. Available at: https://www.guysandstthomas.nhs.uk/resources/patient-information/surgery/orthopaedics/spinal-injections.pdf. Accessed June 2020.